1 Identifying and describing gross lesions
The discipline of pathology is the study of the changes occurring in tissues during disease, including both the morphologic or cellular changes (which we call “lesions”) and molecular abnormalities. Pathology also addresses the causes and mechanisms by which these abnormalities develop, and their functional consequences.
Veterinarians need knowledge of pathology for at least two reasons: on a conceptual level to understand how disease develops, and how changes in tissues form the basis for the clinical appearance of a disease; and on a practical level by observing and interpreting lesions to establish a diagnosis. Postmortem diagnosis is useful to guide the treatment and management of the surviving animals at risk, to provide closure for owners of animals that have died unexpectedly, and to provide factual information and expert opinion on legal, insurance and animal welfare cases. These findings are also useful to the veterinarian: postmortem examination is a method of quality control to monitor the accuracy of clinical diagnosis, and especially for new graduates it provides continuing education on their own cases, and satisfies our curiosity about the basis for the illness in our patients. Finally, postmortem examination is important for discovery and recognition of new diseases, and advancement of the science of veterinary medicine.
Recognition and interpretation of gross lesions is best done methodically. Experienced veterinarians might sometimes glance at a lesion and immediately recognize a probable cause, because they have seen the lesion several times before. However, at an earlier stage of learning—or for cases with atypical or unusual lesions—it is important that you take a more regimented and rigorous approach. This allows us to systematically consider all of the likely possibilities, and then acquire more information that allows us to eliminate some possibilities and further investigate the others. It is sloppy and intellectually lazy to haphazardly examine diseased tissue and make a quick interpretation. It leads to tunnel vision, and we overlook important possibilities or differential diagnoses. Instead, examine diseased tissues carefully, then follow this step-wise approach to interpreting the observations. It is a more rigorous approach to diagnosis, a recipe for success.
It should be obvious that these methods are not unique to pathology, since exactly the same investigative approach is used in other medical disciplines. The general approach to evaluating tissue specimens is similar to other aspects of clinical investigation, and is summarized as follows.
How to investigate gross lesions
1. Identify the lesions
- Identify the tissue and normal structures
- Recognize artefacts and incidental findings
- Identify the main abnormality
2. Describe the lesion
3. Interpret the lesions
- Infer the pathologic process
- Construct a morphologic diagnosis
4. Interpret the likely cause, clinical appearance, histologic correlates, pathogenesis
Identify the lesions
Careful observation is at the heart of pathology, as it is for many other disciplines. It is a skill that is developed with practice and aided by knowledge, but requires commitment and focus. A quick visual observation from a distance is a flimsy basis for making a diagnosis. Observe closely and carefully, using vision and palpation (and even smell), and compare these observations to what you expect in the normal tissue.
A lesion is any observable abnormality in a tissue that occurred before death. Detecting and describing lesions is the critical first step in investigating how the lesion happened, its functional significance, and its cause. Determining that a lesion even exists is not always easy. Perhaps it is a variant of normal? Perhaps it’s not a lesion but something that developed after death? I often grapple with these questions, and you will too. It requires knowledge of the normal appearances of the tissue, and of the tissue changes that commonly occur after death. Only then can we be confident that a tissue differs from normal.
Identify the tissue, and normal structures within the tissue
Knowledge of anatomy and histology is required to identify and interpret lesions. We must be able to identify the organ or tissue we are looking at, and anatomic structures such as cortex, medulla, bronchi, bile ducts and blood vessels. “Chapter 4: Atlas of some normal organs” shows some images of normal tissues, but careful observation of real tissues is the best way to become familiar with their appearance. Whenever you get a chance to look at tissues, think of their histologic structure and how that relates to the macroscopic appearance you are seeing.
Recognize artefacts and incidental findings
Tissues change in appearance after death. We call these postmortem changes “artefacts” and we must be able to recognize them and distinguish them from “real” antemortem lesions. “Chapter 5: Atlas of some artefacts and incidental findings” shows some of the most common artefacts and incidental findings.
Autolysis is the “self-digestion” of tissues. It develops at different rates in different tissues, being slow in muscle and rapid in intestine. Tissues autolyze quickly in warm weather, and in sheep, pigs and whales where the insulating effect of fleece or fat prevents dissipation of body heat after death. Autolyzed tissues have widespread or sometimes localized areas of softening and pallor, which can be distinguished from antemortem necrosis because the adjacent tissue has no reaction.
Putrefaction is another common postmortem change in which bacteria invade into tissue and begin to digest it. This can induce green-black discoloration of tissue (“pseudomelanosis”) due to the breakdown of blood and formation of iron sulfides. At a later stage, there is dissolution of the tissue, emission of a putrid odour, and gas production.
Gas production by saprophytic bacteria causes emphysema in the subcutaneous tissues and liver, and distention of the gastrointestinal tract with gas. This may even lead to postmortem rupture or displacement of the stomach or intestine, and prolapse of the rectum.
Insect larvae (maggots) colonize carcasses and eagerly help the degradative process. Identifying their species and life stages can help establish the time of death in forensic cases.
Rigor mortis is the post-mortem contraction of striated, smooth and cardiac muscle. Rigor mortis makes the carcass stiff during the 1-6 hours after death, and then dissipates over the following 24-48 hours, although there is much variation depending on the energy reserves of the animal and ambient temperatures.
Hypostatic congestion involves the gravitational pooling of blood after death, depending on the position of the body. This often results in reddening of the “down” lung, while the more elevated lung remains of normal colour.
As blood vessels dilate after death, there is pooling of blood within viscera, causing red-purple discoloration of the intestines, lungs and sometimes other tissues. This blood pooling may be uniform within a tissue, or some areas may be blanched due to the pressure of adjacent viscera.
Imbibition of blood or bile pigments results in discoloration of tissues. Hemoglobin imbibition is commonly seen in carcasses subjected to freezing and thawing, and in autolysed fetuses. This breakdown of red blood cells and diffusion of hemoglobin causes red staining of tissues and of fluids in body cavities. The yellow-green-black discoloration of bile imbibition is particularly evident in areas of liver and loops of bowel that contact the gall bladder.
Postmortem trauma (abrasions, fractures) can be differentiated from that sustained during life by the absence of hemorrhage or an inflammatory reaction. Similarly, postmortem scavenging lacks evidence of adjacent tissue hemorrhage, and selectively affects those tissues that are tastiest for scavengers or most easily consumed: the eyes, rectum and external genitalia.
Feed material in the airways – nasal cavity, trachea or bronchi – of ruminants is a consequence of regurgitation of rumen content at the time of death.
Learning to recognize these artefacts within tissues, and distinguish them from the changes that occurred before death are an essential part of the diagnostic process.
Incidental findings are antemortem lesions that are of no functional consequence. We mention them in pathology reports, but we don’t consider them as the likely cause of death, and keep searching for the “true” important lesion that is the cause of death or the basis for the clinical problem.
Common incidental findings will be covered in more detail in the Systems Pathology course (Phase III). A few include: calculus on the teeth, tiny blood-filled nodules on the atrioventricular valves, minor epicardial or endocardial hemorrhages, involution of the thymus, tiny foci of metaplastic bone in the lung, pleural adhesions, siderotic plaques on the splenic capsule, fissures at the edge of the liver, minor ulcers of the margo plicatus in horses, and mesenteric fat necrosis in cows.
Consider three questions when identifying abnormalities in tissues:
1. Is it a normal anatomic structure?
2. Is it a postmortem artefact?
3. Is it different from the normal tissue?
Identify the abnormality
Don’t rush to the description. Instead, take time to observe the tissue and consider how it differs from normal, and whether the change is a postmortem artefact or a “real” antemortem lesion. There is no easy way to develop this skill except with practice, and with open discussion of why a change in the tissue is considered normal, artefact, or a true lesion. It goes without saying that it is critical to correctly identify the abnormality: if you interpret an artefact as a real antemortem lesion, or if you consider a real lesion as normal or an artefact, then the rest of the diagnostic process will be flawed.
Describe the lesions
Description is the basis for scientific communication, by which we are able to share information about lesions or diseases. Description is the basis of the pathology report, which forms the legal record and archive of the findings. Description allows the veterinarian to discuss cases with colleagues, and is an essential element when submitting tissues to diagnostic laboratory. Perhaps most importantly, the act of description focuses and deepens our observations, allowing us to observe things missed by a cursory examination. Description rocks.
In gross (macroscopic) pathology, lesions are described in terms of their location, distribution, size, extent, shape, contour, colour, texture and strength.
Key Point
Different individuals have diverse styles for writing pathology descriptions. Here are a few guidelines and norms to get you started:
- A convention is to not describe normal features or the normal appearance of a tissue, unless there is a specific reason to do so.
- If multiple types of lesions are present, describe one at a time.
- We usually describe the most important abnormalities first, and describe artefactual changes last, if at all. Arguably, this may introduce subjectivity to an otherwise objective factual description, but such reports are more easily understood by the reader.
- Descriptions generally start with an overview of the location and distribution of the lesion. Use the next sentence to communicate the fine details of the lesion’s size, shape, colour, texture, etc.
- Describe lesions using common English words plus anatomic terms. On the other hand, most “pathology words” (e.g. necrosis, hemorrhage, infarct) are only used in the interpretation or diagnosis, not the description.
- Use present tense, to describe what you see before you.
- Avoid abbreviations, as they can be a barrier to those reading your narrative. Abbreviations well known to you may be unknown to others, or have a different meaning.
Please recognize that description must be objective and factual, not subjective, judgemental or interpretive. We are simply recording what is present without offering an opinion on its significance or cause. It is sometimes inefficient or difficult to be completely objective when writing the description. However, at least initially, it is best to describe lesions objectively because these statements of fact cannot be proven wrong. In this way, the description is the statement of the facts, whereas the purity of these truths is tainted if they are mixed with interpretations and inferences. In theory, an observant lay person (if they had knowledge of anatomy and of the appearance of normal tissues) should be as effective in writing a pathology description as an experienced pathologist. In contrast, your interpretation of the lesions is a subjective inference that requires insight, knowledge, judgement and experience. The interpretation is where your knowledge and experience in veterinary pathology and of veterinary medicine is put to use, but this interpretation will often the wrong when you are getting started, and even seasoned experts make incorrect interpretations and judgements about cases. Your objective description of the facts ought to be correct, if you can keep them separate from your interpretation of the findings.
Craft your description to clearly communicate the findings, and allow the reader to develop a clear mental picture of the lesion. It is a narrative that reflects your art of communication. The subsequent sections list the elements of a description (location, distribution, size and extent, colour, texture and strength), but please recognize that:
(a) Some of these descriptive elements may not be applicable to the lesion you are describing.
(b) Simply listing these descriptive elements does not effectively communicate the appearance to the reader. Great authors of modern literature don’t describe their scene with bullet points.
(c) The goal is to communicate the abnormality to the reader, not to simply re-create the visual appearance in words. We don’t want to “paint by dots” or describe what you are seeing on a “pixel by pixel” basis.
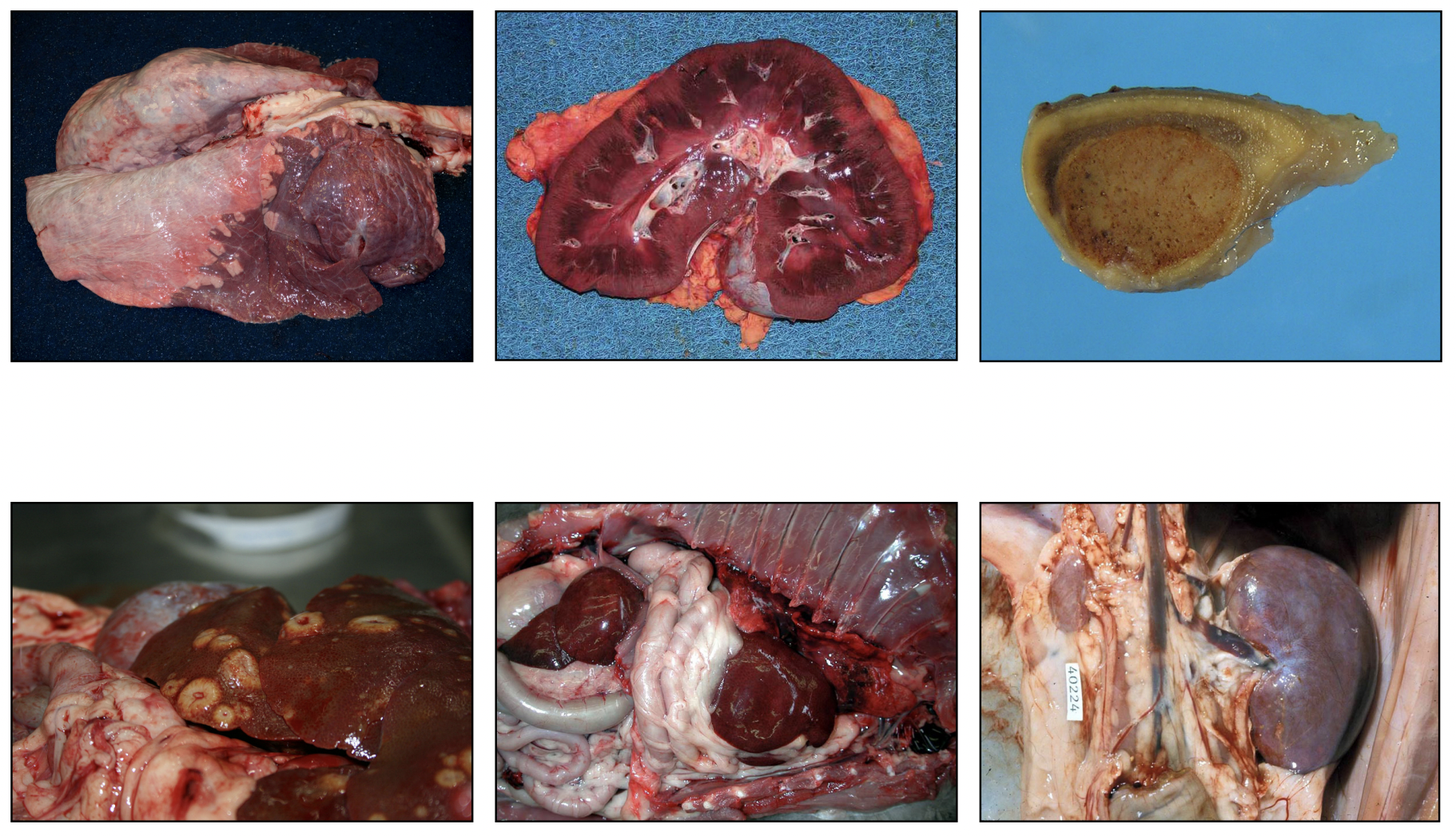
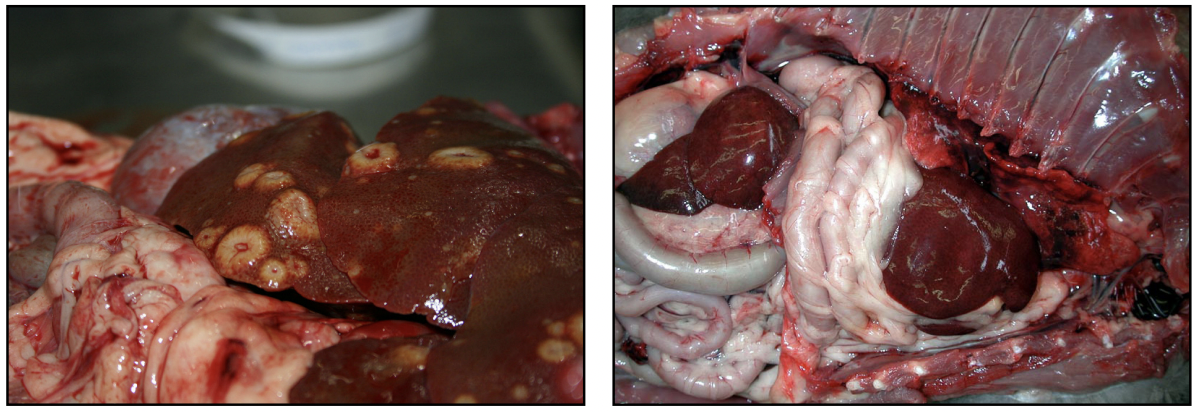
In the left image below, which of the following is more informative to the reader?
“A brown thing with some scattered yellow things”
“Multiple nodules throughout the liver” ?
In the right image below, here is a description that lists some facts but completely fails to communicate the finding: “There is a pink structure at the right, then a brown-purple mass, then some white tubes, then a pale purple-brown membrane, then another brown-purple mass“. We can more effectively communicate the observations as “Cranial to the diaphragm, the pleural cavity contains small intestine, mesentery and a liver lobe, in addition to the lung and heart“. Think about what you are observing, collect those thoughts and step back, and then consider the best approach to communicating that observation.
Descriptions should be concise. The skill of concise description improves with practice, and involves describing the essential features of a lesion without wasting ink on unnecessary words that don’t add useful information or meaning. This skill will serve you well by allowing you to write records, reports, and laboratory submissions quickly but with the necessary details included.
A description should define and clearly communicate the significant morphologic abnormalities in a tissue. This clear written “picture” should allow those reading your report to visualize the lesion and even formulate a morphological diagnosis without having actually seen the specimen.
Although descriptions usually mention the location, distribution, size, extent, shape, contour, colour, texture and strength of lesions, not all of these features are relevant for every lesion. Omit those elements that are not relevant to the lesion you are describing.
Example
Location & distribution | Size & extent | Shape & contour | Colour | Texture & strength
The kidney contains a single localized lesion that extends from mid-medulla to the capsular surface, is 1 x 2 cm diameter, affects 5% of the renal tissue, and is triangular with the apex in the medulla. It is well-demarcated, flat, white-tan with a red margin, and softer than but retains the strength of the adjacent tissue.
Close your eyes. Can you picture the lesion, from the description?
*** Then, compare to the photo of this kidney, shown below ***
Location
State the name of the affected organ or tissue. Wherever possible, precisely specify the location of the lesion; for example, in the renal cortex, pleura, white matter of the parietal lobe of the cerebrum, periphery of the right middle lung lobe, or septal cusp of the left atrioventricular valve. Describe the lesion’s proximity to anatomic structures, such as the bronchi, or a tendency to track along mesenteric blood vessels, or that part of the liver adjacent to the stomach. Lesions in the digestive tract may have a mucosal or serosal location, or are transmural if they involve all layers. Be as precise as you can in specifying the anatomic location, because this can give an important clue to pathogenesis.
Any abnormalities of position should be noted.
Descriptors of location include cranial, rostral and caudal; ventral and dorsal; left and right; lateral and medial; axial and abaxial; central and peripheral; and superficial and deep. You can use plain English words for your descriptions, but these anatomic terms are more concise and precise.
Distribution
The distribution of the lesion is often the single most useful observation, giving valuable insight into the cause. Terms to describe the distribution of lesions are common English words, but they carry some precise meaning that you might not have previously considered, as illustrated in the following diagrams.
Generalized is the opposite of localized. Generalized lesions are present in all parts or all regions of an organ, either affecting the organ entirely (diffuse) or with some remaining normal tissue (multifocal or zonal or patchy lesions).
Diffuse is the opposite of multifocal. Diffuse lesions are uniform throughout, like gas diffusing into a room. It’s useful to emphasize the difference between generalized and diffuse, as illustrated in the diagram below. Diffuse lesions could be generalized (top left image, all areas of the organ are entirely affected) or localized (top centre and right images; one area of the organ is entirely or uniformly affected). Words like patchy, mottled and dappled are sometimes used to describe lesions that affect all areas of an organ, but haven’t yet affected all of the tissue.
Multifocal refers to multiple spots within an organ. Think of polka-dots, although multifocal lesions can be well-demarcated or poorly demarcated. Multifocal lesions that abut each other can be called coalescing. Many multifocal lesions have a random distribution in an organ, but they could be non-random if they consistently affect one microscopic part of the organ.
Focal, localized and locally extensive (or sometimes regionally extensive) have overlapping meaning. In general, a focal lesion is small, while localized or locally extensive lesions are larger or occupy a greater proportion of that area of the organ.
Zonal is a non-random distribution in which the affected tissue repeatedly involves one zone or subcomponent of an organ. It is mainly used to describe lesions in the centrilobular (periacinar) or portal/periportal zones of the liver.
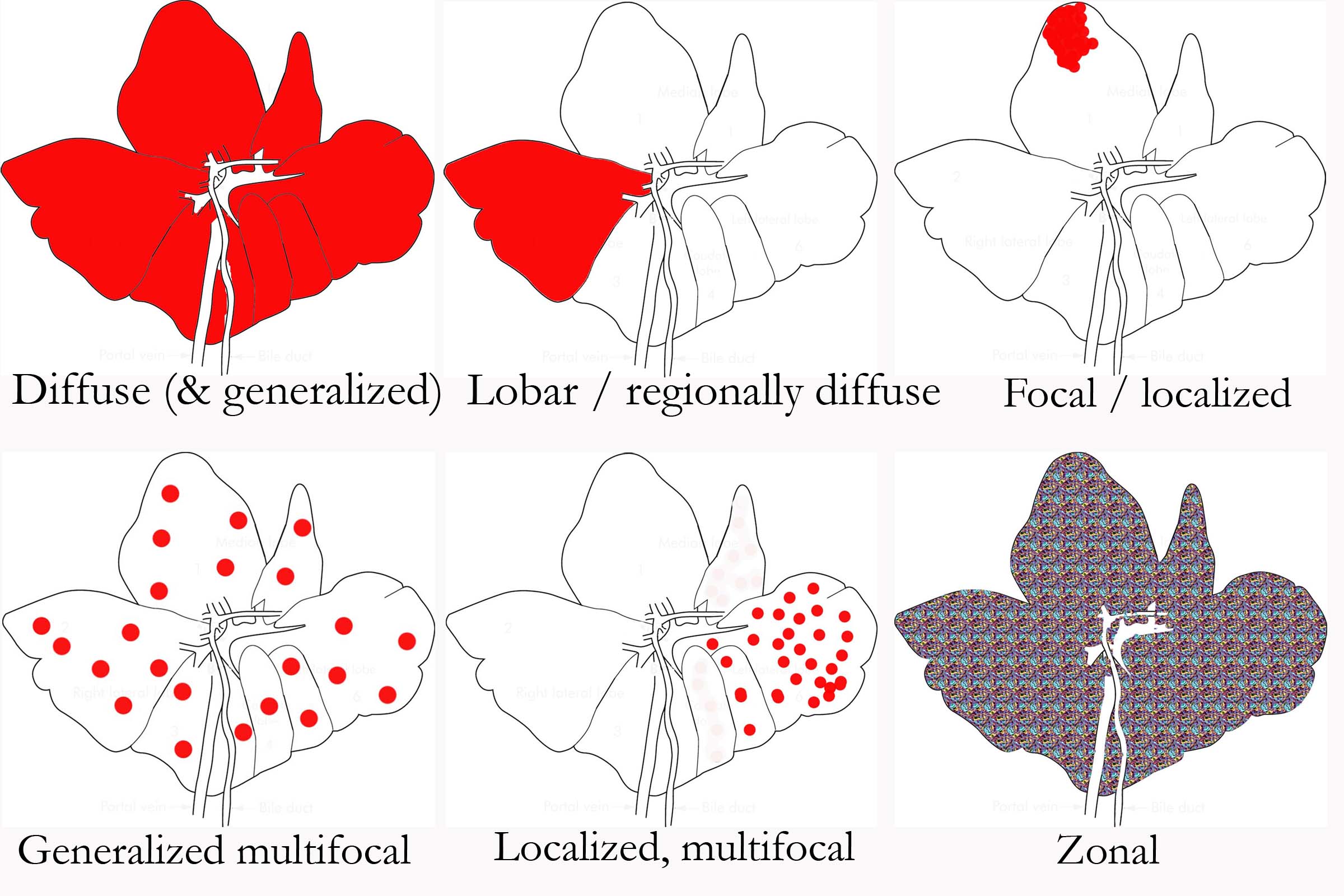
If the anatomic basis for a lesion’s location and distribution is evident, this should be described because it is sure to be a clue to pathogenesis. For example, lesions might affect cortex vs medulla, or follow the course of blood or lymphatic vessels (or bile ducts or bronchioles). In lung and liver, a lobar/lobular distribution affects some lobes/lobules entirely but spares others. A segmental lesion affects a segment or a length of a tubular organ (e.g., intestine) and suggests a localized insult or a vascular basis for the disease. Radially arranged lesions in the renal cortex suggest they are based on the arcuate blood supply or the cause has arrived via the collecting ducts.
In paired or symmetrical organs (kidney, brain, etc.), lesions may be unilateral or bilateral, and symmetrical or asymmetrical.
Key Point
As seen from a distance, lesions may be localized to one lobe of the liver, or generalized throughout all lobes. Localized and generalized are thus opposites.
In terms of the “close-up” distribution of lesions within the affected part of the tissues, the lesion is said to be:
-
- diffuse if it is uniformly affects the tissue, like gas diffusing into a room
- focal or multifocal if the lesions comprise well or poorly demarcated spots or nodules
- zonal if the distribution is non-random and corresponds to a repeating anatomic structure. This is mainly used for liver (eg. lesions in the centrilobular zone of all liver lobules).

Size & extent
The size of lesions, unlike colour or distribution, does not usually give much insight into the cause, but communicates the appearance to the reader. Describe size using metric (SI) units. Do not describe lesions in terms of relationship to familiar objects, because these objects may vary in size (“the size of an apple”) or your audience may not be familiar with them (“the size of a sliotar” would be understood by every vet student at University College Dublin, but not at the Ontario Veterinary College). When lesions range in size, describe the minimum and maximum sizes; for example, “1-3 cm diameter nodules”. We usually don’t need precise measurements when the purpose is to describe the overall appearance to the reader, and lesion size is estimated in this circumstance. Use a ruler only when an exact record of the lesion size is required. Uniformity in size can be mentioned.
Describe the number of lesions present, but recognize that the exact number usually carries little value. “About 30” or “innumberable” is generally sufficient.
The extent of a lesion can be expressed as the percent of the organ (or part of the organ) that is affected. For some organs such as lung, liver, kidney, this is a key predictor of functional significance. One can provide a magnificent description of a lesion, yet fail to mention that it involves only 1% of the organ and is thus unlikely to have any functional significance.
Shape, demarcation & contour
The shape of lesions is usually described in simple geometric terms, such as spherical/circular, rectangular, diamond-shaped, triangular, ovoid, elliptical, linear, serpentine, map-like (or geographic, resembling countries on a map), or irregular. Shape is occasionally informative. For example, triangular or diamond-shaped other sharply angular lesions may be infarcts, or they may have a basis in the lobular anatomy of the organ. Linear or serpentine lesions might follow the course of septa within an organ. Or, serpentine lesions might be larval migration tracks.
Focal or multifocal lesions are described as well-demarcated or poorly demarcated. Well-demarcated lesions might be a tumour that is expansile rather than infiltrative, or lesion that is restricted to an anatomic structure such as a lung lobule, or an infarct defined by the vascular supply to the area, or a distinct structure such as a parasitic cyst. Poorly demarcated lesions could be invasive neoplasms, or infections that are spreading within the tissue.
Surface contour is usually essential for interpreting the underlying processes. Don’t neglect to consider the surface contour! In general, raised areas imply that something has been added to the tissue, such as cells (inflammation, hyperplasia, neoplasia), fluid (edema or blood), or gas (due to bacterial growth in tissues). Depression of the surface below that of the adjacent tissue is usually the result of fibrosis, or loss of tissue such as from atrophy or necrosis. Many lesions of necrosis have a flat surface contour, which may represent no change in tissue volume, or simply a change that cannot be detected grossly. Other fun words to describe the surface contour include bulging, nodular (a raised mass), exophytic (abruptly protruding), sessile (attached to the organ by a broad base), pedunculated (attached by a narrow stalk), papillated (shaggy), villous (finger-like), rugose, corrugated, fissured, serrated, pitted, cavitated, or sunken.
Key Point
The SIZE of the lesions should be QUANTIFIED, by stating the percentage of the organ or tissue affected, the number of lesions, their approximate diameter expressed as a range or as an average, and/or the weight of the affected tissue.
Colour
The colour of a lesion is relatively easy to describe. Tan, white, red, yellow, black and tan are the most commonly encountered colours in both healthy and diseased tissue. Avoid using the suffix “-ish”: if a lesion is not quite white, saying “white-ish” does not give us any guidance as to the direction in which this lesion deviates from the ideal of white. “Tan-white” or beige might better communicate the actual colour. More refined indicators of colour can be useful: amber, bronze, ochre, olive, coffee, and ecru are more precise than “tan”, although it should be recognized that these names may be interpreted differently by others, and a visit to any paint store will prove that this approach can be overdone. I have seen lung lesions the colour of “Old Claret” paint, but that name wouldn’t much help me to imagine the appearance.
The perception of colour is also influenced by how closely one examines the change. A liver might looks orange from a distance, but closer inspection reveals alternating zones of red and tan. This precise observation is surely more informative of the cause. Since colour change often is not uniform, some handy adjectives include variegated, mottled, marbled, and coalescing.
Colour potentially carries information about the nature of the pathologic process. In general, red is the colour imparted to tissue by increased amounts of hemoglobin such as in areas of hemorrhage (focal) or congestion or hyperemia (diffuse). White can indicate the presence of inflammation, neoplasia, necrosis, fibrosis, or mineral deposits. Yellow may also indicate inflammation (pus), bilirubin (icterus), lipid (fatty liver), or fibrin (on the surface of an organ). Green colouration may be seen with bile pigment, eosinophilic inflammation, necrosis (gangrene), some algal or fungal infections, hemosiderin (hemoglobin breakdown products), or putrefaction. Black colouration may indicate the presence of melanin, blood (hypoxic blood or hemoglobin breakdown pigment), necrosis, trematode pigment, exogenous carbon or hydrogen sulfide (from the gastrointestinal tract). These are described further in Chapter 3: Description as a basis for interpretation.
Texture & strength
Descriptors of consistency include those that estimate the firmness of a tissue, and those that estimate the strength. While there is a tendency to equate firm with strong, and soft with weak, this is clearly not true. Fishing net is soft and pliable, yet very strong. A soda cracker is firm, but crumbles easily.
These descriptive words are usually used in the context of the adjacent normal tissue, since a lesion described as firm when found in lung or liver would likely be perceived as soft if it were to occur in bone. In general, increasing degrees of tissue hardness can be described as soft, rubbery, firm, and hard; although the meaning of these terms will differ from one person to the next. Dr. Paul Stromberg (Ohio State University) usefully proposed the following reference points: soft = lips, firm = nose, and hard = forehead.
Other adjectives describing tissue texture may be useful. Turgid is a type of firmness that is due to an internal fluid pressure. Abscesses, for example, may feel turgid yet collapse readily when incised. Gritty texture suggests mineralization. Caseous lesions — resembling feta cheese—are crumbly and somewhat dry. Elastic material on a surface is usually fibrin. Spongy lesions usually contain multiple pockets filled with air or sometimes fluid. The texture of fluids may be described as watery, viscid, mucoid, gelatinous, creamy, clotted, or inspissated.
The strength of tissue must always be judged by the cut surface, as it is obscured by the fibrous capsule. Tissue strength may be described as friable if it is weak and breaks apart easily, or tough if it has greater than normal strength. Loss of tissue strength (or, being friable) is the most reliable and consistent indicator of necrosis. A tissue that is tougher than normal usually contains fibrous tissue (scarring). A liver with hepatic lipidosis feels quite firm, yet breaks apart readily once you apply some digital pressure to the cut surface; it is thus “firm but friable”.
Descriptive terms
1. Location & distribution
2. Size & extent
3. Shape, demarcation & contour
4. Colour
5. Texture & strength
This completes the section on lesion description. Describing a lesion communicates its appearance to others, and makes an accurate record of what we observed. Describing a lesion also forces us to better observe and think carefully about the lesion. It is the essential basis for interpreting lesions. If we are not effective at describing a lesion, or if we can’t be bothered to do so, it often limits our ability to properly interpret the lesion and investigate its cause and significance. Such self-inflicted failure is painful. Description is an essential step in pathology problem-solving. Learn to describe, and be happy!

