9.9 Pressures in the Body
Learning Objectives
By the end of this section, you will be able to:
- Explain the concept of pressure the in human body.
- Explain systolic and diastolic blood pressures.
- Describe pressures in the eye, lungs, spinal column, bladder, and skeletal system.
Pressure in the Body
Next to taking a person’s temperature and weight, measuring blood pressure is the most common of all medical examinations. Control of high blood pressure is largely responsible for the significant decreases in heart attack and stroke fatalities achieved in the last three decades. The pressures in various parts of the body can be measured and often provide valuable medical indicators. In this section, we consider a few examples together with some of the physics that accompanies them.
Table 9.5 lists some of the measured pressures in mm Hg, the units most commonly quoted.
| Body system | Gauge pressure in mm Hg |
|---|---|
| Blood pressures in large arteries (resting) | |
| Maximum (systolic) | 100–140 |
| Minimum (diastolic) | 60–90 |
| Blood pressure in large veins | 4–15 |
| Eye | 12–24 |
| Brain and spinal fluid (lying down) | 5–12 |
| Bladder | |
| While filling | 0–25 |
| When full | 100–150 |
| Chest cavity between lungs and ribs | −8 to −4 |
| Inside lungs | −2 to +3 |
| Digestive tract | |
| Esophagus | −2 |
| Stomach | 0–20 |
| Intestines | 10–20 |
| Middle ear | 1 |
Blood Pressure
Common arterial blood pressure measurements typically produce values of 120 mm Hg and 80 mm Hg, respectively, for systolic and diastolic pressures. Both pressures have health implications. When systolic pressure is chronically high, the risk of stroke and heart attack is increased. If, however, it is too low, fainting is a problem. Systolic pressure increases dramatically during exercise to increase blood flow and returns to normal afterward. This change produces no ill effects and, in fact, may be beneficial to the tone of the circulatory system. Diastolic pressure can be an indicator of fluid balance. When low, it may indicate that a person is hemorrhaging internally and needs a transfusion. Conversely, high diastolic pressure indicates a ballooning of the blood vessels, which may be due to the transfusion of too much fluid into the circulatory system. High diastolic pressure is also an indication that blood vessels are not dilating properly to pass blood through. This can seriously strain the heart in its attempt to pump blood.
Blood leaves the heart at about 120 mm Hg but its pressure continues to decrease (to almost 0) as it goes from the aorta to smaller arteries to small veins (see Figure 9.34). The pressure differences in the circulation system are caused by blood flow through the system as well as the position of the person. For a person standing up, the pressure in the feet will be larger than at the heart due to the weight of the blood [latex]\left(\right. P = hρg \left.\right)[/latex]. If we assume that the distance between the heart and the feet of a person in an upright position is 1.4 m, then the increase in pressure in the feet relative to that in the heart (for a static column of blood) is given by
[latex]\begin{align*}Δ P &= Δ hρg \\ &= \left(1.4 m\right) \left(\text{1050 kg} /\text{m}^{3}\right) \left(9.80 m /\text{s}^{2}\right) \\ &= 1 . 4 \times \text{10}^{4} \text{Pa} \\ &= \text{108 mm Hg} .\end{align*}[/latex]
Increase in Pressure in the Feet of a Person
[latex]\begin{align*}Δ P &= Δ hρg \\ &= \left(1.4 m\right) \left(\text{1050 kg} /\text{m}^{3}\right) \left(9.80 m /\text{s}^{2}\right) \\ &= 1 . 4 \times \text{10}^{4} \text{Pa} \\ &= \text{108 mm Hg} .\end{align*}[/latex]
Standing a long time can lead to an accumulation of blood in the legs and swelling. This is the reason why soldiers who are required to stand still for long periods of time have been known to faint. Elastic bandages around the calf can help prevent this accumulation and can also help provide increased pressure to enable the veins to send blood back up to the heart. For similar reasons, doctors recommend tight stockings for long-haul flights.
Blood pressure may also be measured in the major veins, the heart chambers, arteries to the brain, and the lungs. But these pressures are usually only monitored during surgery or for patients in intensive care since the measurements are invasive. To obtain these pressure measurements, qualified health care workers thread thin tubes, called catheters, into appropriate locations to transmit pressures to external measuring devices.
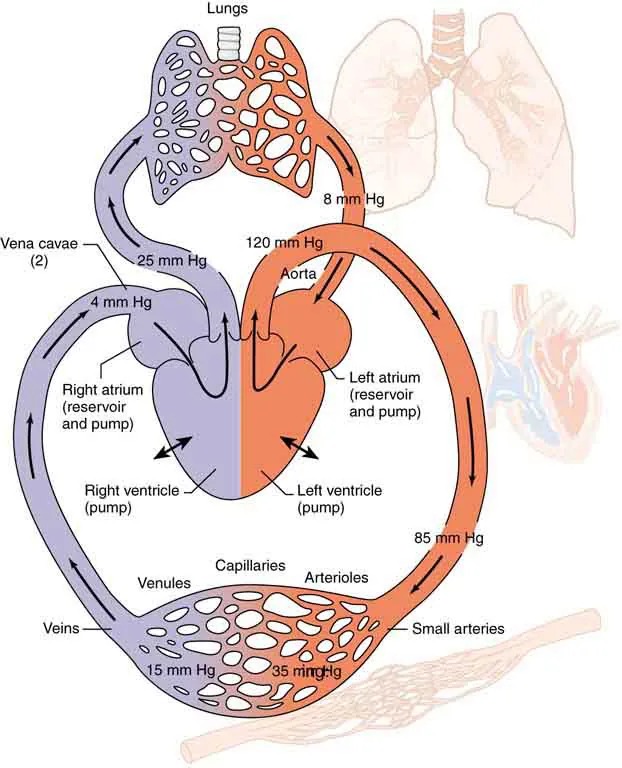
The heart consists of two pumps—the right side forcing blood through the lungs and the left causing blood to flow through the rest of the body (Figure 9.34). Right-heart failure, for example, results in a rise in the pressure in the vena cavae and a drop in pressure in the arteries to the lungs. Left-heart failure results in a rise in the pressure entering the left side of the heart and a drop in aortal pressure. Implications of these and other pressures on flow in the circulatory system will be discussed in more detail in Fluid Dynamics and Its Biological and Medical Applications.
Two Pumps of the Heart
The heart consists of two pumps—the right side forcing blood through the lungs and the left causing blood to flow through the rest of the body.
Fluid Dynamics and Its Biological and Medical Applications
Figure 9.34 Schematic of the circulatory system showing typical pressures. The two pumps in the heart increase pressure and that pressure is reduced as the blood flows through the body. Long-term deviations from these pressures have medical implications discussed in some detail in the . Only aortal or arterial blood pressure can be measured noninvasively. Image from OpenStax College Physics 2e, CC-BY 4.0
Image Description
The image is a diagram of the human cardiovascular system, illustrating the flow of blood through the heart, lungs, and body. The heart is at the center, divided into two sides: the right side is shaded purple, and the left side is shaded red. Key areas are labeled with the blood pressure in millimeters of mercury (mm Hg) for various parts of the circulatory system.
On the right side, the pathway is as follows:
- Blood enters the right atrium, labeled as a “reservoir and pump,” at 4 mm Hg.
- Blood then moves to the right ventricle, labeled as a “pump.” It travels through the pulmonary arteries to the lungs, where the pressure is marked as 25 mm Hg.
- After oxygenation in the lungs, the blood returns to the left side of the heart via the pulmonary veins at 8 mm Hg.
On the left side, the pathway is as follows:
- Blood from the lungs enters the left atrium, labeled as a “reservoir and pump.”
- Blood flows into the left ventricle, labeled as a “pump,” and then is pushed into the aorta at 120 mm Hg.
- The red-shaded area routes blood through small arteries and arterioles, marked with pressures of 85 mm Hg and 35 mm Hg, respectively.
- This blood travels through the capillaries, venules, and veins, returning to the right atrium with a pressure of 15 mm Hg.
The diagram includes labels like “vena cavae,” “capillaries,” “venules,” “arterioles,” “small arteries,” and “veins,” indicating various components of the circulatory system involved in the transportation of blood.
Pressure in the Eye
The shape of the eye is maintained by fluid pressure, called intraocular pressure, which is normally in the range of 12.0 to 24.0 mm Hg. When the circulation of fluid in the eye is blocked, it can lead to a buildup in pressure, a condition called glaucoma. The net pressure can become as great as 85.0 mm Hg, an abnormally large pressure that can permanently damage the optic nerve. To get an idea of the force involved, suppose the back of the eye has an area of [latex]6 . 0 \text{cm}^{2}[/latex], and the net pressure is 85.0 mm Hg. Force is given by [latex]F = \text{PA}[/latex]. To get [latex]F[/latex] in newtons, we convert the area to [latex]\text{m}^{2}[/latex] ([latex]\text{1 m}^{2} = \text{10}^{4} \text{cm}^{2}[/latex]). Then we calculate as follows:
[latex]{\small\begin{align*}F &= hρ \text{gA}\\&= \left(85.0 \times \text{10}^{- 3} \text{m}\right) \left(\text{13} . 6 \times \text{10}^{3} \text{kg}/\text{m}^{3}\right) \left(9 . \text{80} \text{m}/\text{s}^{2}\right) \left(6 . 0 \times \text{10}^{- 4} \text{m}^{2}\right)\\&= 6.8 N.\end{align*}}[/latex]
Eye Pressure
The shape of the eye is maintained by fluid pressure, called intraocular pressure. When the circulation of fluid in the eye is blocked, it can lead to a buildup in pressure, a condition called glaucoma. The force is calculated as
[latex]{\scriptsize\begin{align*}F &= hρ \text{gA}\\ &= \left(85.0 \times \text{10}^{- 3} \text{m}\right) \left(\text{13} . 6 \times \text{10}^{3} \text{kg}/\text{m}^{3}\right) \left(9.80 \text{m}/\text{s}^{2}\right) \left(6.0 \times \text{10}^{- 4} \text{m}^{2}\right)\\ &= 6.8 N.\end{align*}}[/latex]
This force is the weight of about a 680-g mass. A mass of 680 g resting on the eye (imagine 1.5 lb resting on your eye) would be sufficient to cause it damage. (A normal force here would be the weight of about 120 g, less than one-quarter of our initial value.)
People over 40 years of age are at greatest risk of developing glaucoma and should have their intraocular pressure tested routinely. Most measurements involve exerting a force on the (anesthetized) eye over some area (a pressure) and observing the eye’s response. A noncontact approach uses a puff of air and a measurement is made of the force needed to indent the eye (Figure 9.35). If the intraocular pressure is high, the eye will deform less and rebound more vigorously than normal. Excessive intraocular pressures can be detected reliably and sometimes controlled effectively.
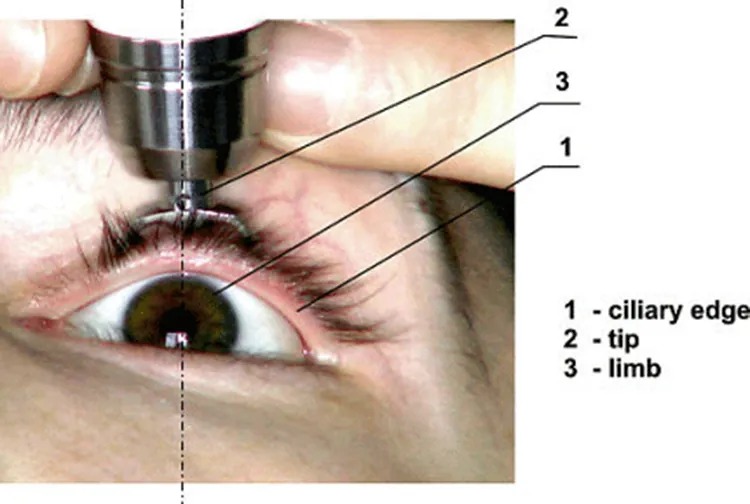
Figure 9.35 The intraocular eye pressure can be read with a tonometer. Image from OpenStax College Physics 2e, CC-BY 4.0
Image Description
The image depicts an eye undergoing a procedure. A tool is being operated near the eye. The hand holding the tool is gently pulling the upper eyelid upwards, revealing the sclera and the upper portion of the iris. Several lines point to specific parts of the eye with labels:
| Number | Label |
|---|---|
| 1 | Ciliary edge |
| 2 | Tip |
| 3 | Limb |
The eye is open wide and the instrument appears to be performing a task near the eyelashes and the upper part of the eyeball. The image is focused on the anatomy and tool placement.
Example 9.13
Calculating Gauge Pressure and Depth: Damage to the Eardrum
Suppose a 3.00-N force can rupture an eardrum. (a) If the eardrum has an area of [latex]1 . \text{00} \text{cm}^{2}[/latex], calculate the maximum tolerable gauge pressure on the eardrum in newtons per meter squared and convert it to millimeters of mercury. (b) At what depth in freshwater would this person’s eardrum rupture, assuming the gauge pressure in the middle ear is zero?
Strategy for (a)
The pressure can be found directly from its definition since we know the force and area. We are looking for the gauge pressure.
Solution for (a)
[latex]\begin{align*}P_{\text{g}} &= F / A \\&= 3 . \text{00} \text{N} / \left(\right. 1 . \text{00} \times \text{10}^{- 4} \text{m}^{2} \left.\right)\\ &= 3 . \text{00} \times \text{10}^{4} \text{N}/\text{m}^{2} .\end{align*}[/latex]
We now need to convert this to units of mm Hg:
[latex]P_{\text{g}} = 3 . 0 \times \text{10}^{4} \text{N}/\text{m}^{2} \left(\frac{1.0 mm Hg}{\text{133} \text{N}/\text{m}^{2}}\right) = \text{226 mm Hg}.[/latex]
Strategy for (b)
Here we will use the fact that the water pressure varies linearly with depth [latex]h[/latex] below the surface.
Solution for (b)
[latex]P = hρg[/latex] and therefore [latex]h = P / ρg[/latex]. Using the value above for [latex]P[/latex], we have
[latex]h = \frac{3.0 \times \text{10}^{4} \text{ N}/\text{m}^{2}}{\left(\right. 1.00 \times \text{10}^{3} \text{ kg}/\text{m}^{3} \left.\right) \left(\right. 9.80 m /\text{s}^{2} \left.\right)} = 3.06 m.[/latex]
Discussion
Similarly, increased pressure exerted upon the eardrum from the middle ear can arise when an infection causes a fluid buildup.
Pressure Associated with the Lungs
The pressure inside the lungs increases and decreases with each breath. The pressure drops to below atmospheric pressure (negative gauge pressure) when you inhale, causing air to flow into the lungs. It increases above atmospheric pressure (positive gauge pressure) when you exhale, forcing air out.
Lung pressure is controlled by several mechanisms. Muscle action in the diaphragm and rib cage is necessary for inhalation; this muscle action increases the volume of the lungs thereby reducing the pressure within them Figure 9.36. Surface tension in the alveoli creates a positive pressure opposing inhalation. (See 9.8 Cohesion and Adhesion in Liquids: Surface Tension and Capillary Action.) You can exhale without muscle action by letting surface tension in the alveoli create its own positive pressure. Muscle action can add to this positive pressure to produce forced exhalation, such as when you blow up a balloon, blow out a candle, or cough.
The lungs, in fact, would collapse due to the surface tension in the alveoli, if they were not attached to the inside of the chest wall by liquid adhesion. The gauge pressure in the liquid attaching the lungs to the inside of the chest wall is thus negative, ranging from [latex]- 4[/latex] to [latex]- 8 mm Hg[/latex] during exhalation and inhalation, respectively. If air is allowed to enter the chest cavity, it breaks the attachment, and one or both lungs may collapse. Suction is applied to the chest cavity of surgery patients and trauma victims to reestablish negative pressure and inflate the lungs.
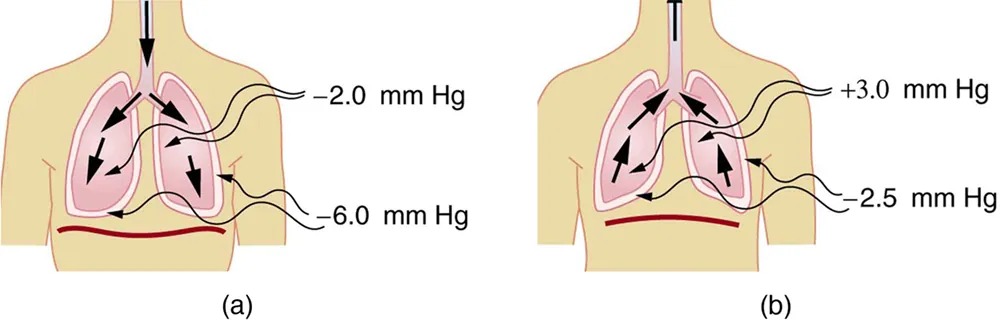
Figure 9.36 (a) During inhalation, muscles expand the chest, and the diaphragm moves downward, reducing pressure inside the lungs to less than atmospheric (negative gauge pressure). Pressure between the lungs and chest wall is even lower to overcome the positive pressure created by surface tension in the lungs. (b) During gentle exhalation, the muscles simply relax and surface tension in the alveoli creates a positive pressure inside the lungs, forcing air out. Pressure between the chest wall and lungs remains negative to keep them attached to the chest wall, but it is less negative than during inhalation. Image from OpenStax College Physics 2e, CC-BY 4.0
Image Description
The image consists of two diagrams labeled (a) and (b) that depict the pressure differences in the thoracic cavity during the respiratory cycle, highlighting inhalation and exhalation processes.
(a) Inspiration:
- The diagram shows a human torso with lungs, arrows indicating the flow of air into the lungs.
- Pressure annotations are shown with -2.0 mm Hg inside the lungs and -6.0 mm Hg in the pleural cavity, illustrating negative pressure facilitating airflow into the lungs.
- The diaphragm is shown in a flattened position indicating contraction.
(b) Expiration:
- The diagram shows a human torso with lungs, arrows indicating the flow of air out of the lungs.
- Pressure annotations are shown with +3.0 mm Hg inside the lungs and -2.5 mm Hg in the pleural cavity, illustrating positive pressure aiding in expelling air from the lungs.
- The diaphragm is shown in a relaxed, dome-shaped position.
Other Pressures in the Body
Spinal Column and Skull
Normally, there is a 5- to12-mm Hg pressure in the fluid surrounding the brain and filling the spinal column. This cerebrospinal fluid serves many purposes, one of which is to supply flotation to the brain. The buoyant force supplied by the fluid nearly equals the weight of the brain, since their densities are nearly equal. If there is a loss of fluid, the brain rests on the inside of the skull, causing severe headaches, constricted blood flow, and serious damage. Spinal fluid pressure is measured by means of a needle inserted between vertebrae that transmits the pressure to a suitable measuring device.
Bladder Pressure
This bodily pressure is one of which we are often aware. In fact, there is a relationship between our awareness of this pressure and a subsequent increase in it. Bladder pressure climbs steadily from zero to about 25 mm Hg as the bladder fills to its normal capacity of [latex]\text{500} \text{cm}^{3}[/latex]. This pressure triggers the micturition reflex, which stimulates the feeling of needing to urinate. What is more, it also causes muscles around the bladder to contract, raising the pressure to over 100 mm Hg, accentuating the sensation. Coughing, straining, tensing in cold weather, wearing tight clothes, and experiencing simple nervous tension all can increase bladder pressure and trigger this reflex. So can the weight of a pregnant woman’s fetus, especially if it is kicking vigorously or pushing down with its head! Bladder pressure can be measured by a catheter or by inserting a needle through the bladder wall and transmitting the pressure to an appropriate measuring device. One hazard of high bladder pressure (sometimes created by an obstruction), is that such pressure can force urine back into the kidneys, causing potentially severe damage.
Pressures in the Skeletal System
These pressures are the largest in the body, due both to the high values of initial force, and the small areas to which this force is applied, such as in the joints.. For example, when a person lifts an object improperly, a force of 5000 N may be created between vertebrae in the spine, and this may be applied to an area as small as [latex]\text{10} \text{cm}^{2}[/latex]. The pressure created is
[latex]P = F / A = \left(\right. \text{5000 N} \left.\right) / \left(\right. \text{10}^{- 3} \text{m}^{2} \left.\right) = 5.0 \times \text{10}^{6} \text{N}/\text{m}^{2}[/latex] or about 50 atm! This pressure can damage both the spinal discs (the cartilage between vertebrae), as well as the bony vertebrae themselves. Even under normal circumstances, forces between vertebrae in the spine are large enough to create pressures of several atmospheres. Most causes of excessive pressure in the skeletal system can be avoided by lifting properly and avoiding extreme physical activity. (See 7.6 Forces and Torques in Muscles and Joints.)
There are many other interesting and medically significant pressures in the body. For example, pressure caused by various muscle actions drives food and waste through the digestive system. Stomach pressure behaves much like bladder pressure and is tied to the sensation of hunger. Pressure in the relaxed esophagus is normally negative because pressure in the chest cavity is normally negative. Positive pressure in the stomach may thus force acid into the esophagus, causing “heartburn.” Pressure in the middle ear can result in significant force on the eardrum if it differs greatly from atmospheric pressure, such as while scuba diving. The decrease in external pressure is also noticeable during plane flights (due to a decrease in the weight of air above relative to that at the Earth’s surface). The Eustachian tubes connect the middle ear to the throat and allow us to equalize pressure in the middle ear to avoid an imbalance of force on the eardrum.
Many pressures in the human body are associated with the flow of fluids. Fluid flow will be discussed in detail in the Fluid Dynamics and Its Biological and Medical Applications.

