Types of Simulations
Chapter 1: Simulation Modalities
There are many forms of simulators that simulate real scenarios by using a machine or computer program. There are many forms of simulators in nursing education and each type of simulator has been developed to achieve one or more learning objectives. In this chapter, the types of simulation will mainly focus on human patient simulators or manikin-based simulation. Computer based simulation will be discussed later in more detail in the chapter about Virtual Simulation. This chapter is designed to help you understand the types of simulation that are available and provide some context of the distinct language that is used in simulation.
Patient Type
There are four types of patients used in simulators: human, digital, analogue, and electronic patients. The human patient is where a person portrays a particular medical condition. A digital patient is where computer graphic animations are used to represent a patient and medical devices/instrument (Cant et al., 2019). An analogue patient is a partial or full manikin that are either static or moves mechanically. An electronic type of patient is represented in the form of a full or partial body manikin that can be controlled by using a combination of electronic and mechanical means.
Modality
Modality is the term used to refer to the type of simulation methodology used such as standardized patient or full-body manikins. Selecting a specific modality is based on many factors such as the availability of equipment, people, or the lesson objectives (Carey and Rossler, 2020). The design of the simulation scenario depends on the proper identification of the level of fidelity to meet a specific learning objective. The choice of simulation modality is important to have a successful simulation experience.
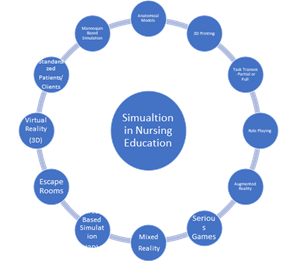
Figure 1: Simulation Modalities Used in Nursing Education
Anatomical Models
Simulation-based education (SBE) has a long and rich history in nursing dating back to 1874 when Florence Nightingale and Florence Lees, in their writings, advocated that nursing schools should use models such as a jointed skeleton and “mechanical dummies” that were arm and leg limbs used for teaching how to bandage. Earlier models of an anatomical pelvis dating to the late 1700s have been found and were used for training midwives (Sanko, 2017). These anatomical models are being increasingly replaced with virtual anatomy tables and virtual reality three dimensional (3D) programs that teach anatomy and allow the participant to virtually dissect a patient (Aebersold, 2018).
Full-Bodied and Partial Body Task Trainers
The most famous and first full-bodied task trainer to be introduced into nursing education was Mrs. Chase in 1910 (Aebersold, 2018; Nehring & Lashley, 2009; Sanko, 2017). Mrs. Chase was the beginning of using full-body manikins as a task trainer to be used by nursing participants to learn clinical skills such as how to “dress, turn and transfer patients” (Aebersold, 2016, p. 2). In 1914, Arabella was created as an upgrade to Mrs. Chase where she was aesthetically modernized, an internal reservoir allowed for catheterization and an injection port to the arm were added.
Mrs. Chase continued to be popular through the 1950s (Sanko, 2017). The 1930s saw the emergence of simulation labs where space was dedicated to practicing nursing skills and became the place where partial and full-bodied task trainers were used to train nursing participants on giving injections, bathing, intravenous insertion, insertion of catheters, and dressing changes (Sanko, 2017).
Low Fidelity Manikins
Low fidelity manikins can be either a full bodied or partial task trainer. These manikins are static or provide a mechanical movement and have no computer technology. These manikins are used for specific tasks such as cardiopulmonary resuscitation which helps the nursing participant build their knowledge (Carey & Rossler, 2020; Park & Shin, 2016). Skills such as injections, dressing changes, or bathing can be easily done with a low-fidelity manikin.
Medium Fidelity Manikins
The medium-fidelity manikins is a full-body manikin that has limited computer technology that allows it to be controlled by an external handheld device (Kim et al., 2016). These manikins are best used for building participant competence for performing skills, tasks, and procedures (Park & Shin, 2016). For example, the manikin can be used for the assessment of heart, breath, and bowel sounds. It can also provide opportunities to insert catheters or nasogastric tubes as it has reservoirs for the bladder and stomach so that participants can be assured of proper placement. It also provides sounds such as coughing, groaning or vomiting. These sounds provide a realistic response to the procedure (intravenous insertion, suctioning, dressing changes, or injections) that the participant is performing.
High Fidelity Manikins
The 1990s to the present day marks the modern era of simulation in nursing education with the adoption of human patient simulators or manikin-based simulation. Medical technology companies such as Laerdal, CAE, and Guamard changed the landscape of simulation in the 1990s with the introduction of affordable, computerized high-fidelity manikins.
High Fidelity manikins are full-bodied, computerized, and controlled by a software program that is operated by a simulation facilitator. These manikins offer the highest level of realism related to anatomical structures, communication, and the ability to respond to participant interventions. These manikins can mimic human traits such as but not limited to blinking eyelids, produce tears or sweat, make vocal sounds, produce realistic heart and lung sounds, and peripheral and central pulses (Aebersold, 2018). Since the 1990s the focus of technology companies was to develop better technology within the high-fidelity manikin whereas these new human patient simulators overlay technology onto the manikin. Manikin innovations continue and have brought about new manikins such as ALEX that has speech recognition and response abilities for communication and new companies such as Lifecast Body Simulations, SynDaver, and Echo Healthcare that are placing their focus on providing realism and immersive simulation experiences by making manikins look and feel like humans.
Three Dimensional Printed Manikins
Three-dimensional (3D) printing technology, molding, and casting techniques have provided the opportunity to create a realistic three-dimensional copy of a human body of different ethnicities, ages, weight, body structures, and gender. The use of virtual programs and accessory technology (such as monitors for vital signs) are necessary as the manikin lacks any internal technology. The changes towards realism have improved to such an extent that the label of manikin seems inadequate. The terms high fidelity or human patient simulators provide a more accurate description of what is presently being used in nursing simulation labs across the country.
Three-dimensional (3D) printing technology is one of the latest contributions to simulation. 3D printing has become cheaper and nursing labs can use them to create their own partial task trainers such as injectable pads or anatomical body parts such as limbs for intravenous insertion training (Bassendowski, 2013).
Standardized Patient
The 1960s was the era where simulated role-playing began to evolve into what is now known as standardized patients or clients which are commonly used for healthcare professional assessments in an Objective Structured Clinical Examination (OSCE). Standardized patients were a new simulation teaching strategy created by Howard Burrows M.D. for medical participants to interact with patients for history taking and health assessments (Churchouse & McCafferty, 2012). Standardized patients are trained to represent a patient with a specific medical condition (Carey & Rossler, 2020) as opposed to role-playing when participants explore nurse-patient or interdisciplinary interactions. Those individuals can take on the unscripted role in the scenario. Role-playing can be conducted with tools such as a dialogue exchange or audio-visuals (Nehring & Lashley, 2009).