8.1
Basic Concepts
Recording Dental Images
No film or processing chemistry is used for recording dental images. An electronic sensor and computerized imaging system that produces x-ray images almost instantly on a computer monitor are used.
Terminology
Term |
Definition |
| Analog Image | An image produced on conventional film that looks like (is “analogous to”) the thing it represents. |
| Bit-Depth Image | The number of possible gray-scale combinations for each pixel. |
| Charge-Coupled Device (CCD) | A solid-state silicon chip detector that converts light or x-ray photons into an electrical charge or signal; a CCD is found in the intraoral sensor. |
| Digital Imaging | A filmless imaging system; a method of capturing an image using a sensor, breaking it into electronic pieces, and presenting and storing the image using a computer. |
| Digital Image | An image composed of pixels. |
| Digital Subtraction | One of the features of digital imaging; a method of reversing the gray scale as an image is viewed; radiolucent images (normally black) appear white and radiopaque images (normally white) appear black. |
| Digitize | In digital imaging, to convert an image into digital form that, in turn, can be processed by a computer. |
| Direct Digital Imaging | A method of obtaining a digital image in which an intraoral sensor is exposed to x-radiation to capture an image that can be viewed on a computer monitor. |
| Indirect Digital Imaging | A method of obtaining a digital image from a sensor after exposure to x-rays by using a scanner to convert information into a digital form so that it can be viewed on a computer monitor. |
| Line Pairs/Millimeter (lp/mm) | A measurement used to evaluate the ability of the computer to capture the resolution (or detail) of an image. |
| Pixel | A discrete unit of information; in digital electronic images, digital information is contained in, and presented as, discrete units of information (also known as picture element). |
| Sensor | In digital imaging, a receptor that is used to capture an intraoral or extraoral image. |
| Storage Phosphor Imaging | An indirect method of obtaining a digital image in which the image is recorded on phosphor-coated plates and then placed into an electronic processor, where a laser scans the plate and produces an image on a computer screen. |
Purpose and Use
The purpose of digital imaging is to generate images that can be used in the diagnosis and assessment of dental disease, to detect lesions, diseases, and conditions of the teeth and surrounding structures, to be able to confirm or classify suspected disease, to localize lesions or foreign objects, and to provide information during dental procedures.
More purposes of imaging are to evaluate growth and development, illustrate changes secondary to caries, periodontal disease, or trauma, document the condition of a patient at a specific point in time, and aid in the development of a clinical treatment plan.
Fundamentals
Digital imaging is a method of capturing an image using a sensor, breaking it into electronic pieces, and presenting and storing the image using a computer. Image used to describe the pictures that are produced. A sensor is placed inside the mouth and the electronic signal is digitized. The sensor picks up the x-rays and transmits an image to the computer, which digitizes the image and displays it in seconds.
Here is an image displaying a full-mouth series of digital images displayed on a computer monitor.

Radiation Exposure
Digital imaging requires less x-radiation exposure than film-based imaging. The typical sensor is more sensitive to x-rays than conventional film, and exposure times are 50% to 90% less than that required for conventional radiography.
Practice Makes Perfect
Equipment
X-ray Unit
X-ray unit is the traditional dental radiograph machine that can be used and the timer must be calibrated. Most digital imaging systems use a conventional dental x-ray unit as the x-radiation source. The x-ray unit timer must be adapted to allow exposures in a time frame of 1/100 of a second.
Sensor
A sensor is a small detector that is placed in the mouth of the patient and used to capture the radiographic image. There is wired and wireless. Wired is the imaging sensor is linked by a fiber optic cable to a computer and wireless is the imaging sensor that is not linked by a cable. Most manufacturers produce sensors similar in dimension to size 0, 1, 2, and 4 intraoral films.
The most popular types of direct sensor technologies are charge-coupled devices (CCD), complementary metal oxide semiconductor/active pixel sensors, and charge injection devices.
Intraoral Sensor
 |
 |
| A #2 intraoral film, which is similar in size and shape to a sensor used in digital imaging | A wired sensor used with digital imaging showing the intraoral sensor at one end and the link to the computer at the other end |
Charge-Coupled Device (CCD)
A charge-coupled device is the most common image receptor used in dental digital imaging. It is a solid-state detector that contains a silicon chip with an electronic circuit embedded in it. The electrons that make up the silicon CCD can be visualized as being divided into an arrangement of blocks or picture elements known as pixels. CCD technology is also used in fax machines, home video cameras, microscopes, and telescopes.
A pixel is a small box or “well” into which the electrons produced by the x-ray exposure are deposited. A pixel is the digital equivalent of a silver crystal in conventional radiography. It is also more structured in an ordered arrangement, unlike the random arrangement of silver crystals.
The x-ray photons that come into contact with the CCD cause electrons to be released from the silicon and produce a corresponding electronic charge. Each pixel arrangement, or electron potential well, contains an electronic charge proportional to the number of electrons that reacted within the well. Each electronic well corresponds to a specific area on the linked computer screen.
Complementary Metal Oxide Semiconductor/Active Pixel Sensor (CMOS/APS)
One manufacturer uses a CMOS/APS sensor instead of a CCD and the chip is less expensive to produce and offers greater durability than the CCD. The difference is that it is silicone-based and differs from the CCD in the manner in which the pixels are read. It also claims to have 25% greater resolution.
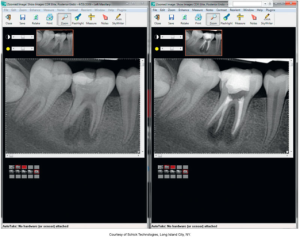
Computer
Computers are used to store the incoming electronic signal and convert the electronic signal from the sensor into a shade of gray that is viewed on the computer monitor. The computer digitizes, processes, and stores information received from the sensor, and an image is recorded on a computer monitor in 0.5 to 120 seconds. It also has a split screen and magnification capability.
The images below show 1. a digital image on a computer monitor of a mandibular right periapical region and 2. a split-screen technology that assists the dental professional in viewing several images of tooth #46 simultaneously.
 |
 |
Types of Digital Imaging
There are two types of digital imaging: direct and indirect digital imaging. The difference between the methods lies in how the image is obtained and in what size the receptor plates are available.
Direct Digital Imaging
Components of direct digital imaging include an intraoral dental x-ray unit, a sensor, and a computer with imaging software. A sensor is placed into the mouth of the patient and exposed. The sensor captures the image and transmits it to the computer monitor. Software is then used to enhance and store the image.
An anterior beam alignment device holds the digital sensor and the wire attachment. The image below is an anterior beam alignment device.

Indirect Digital Imaging
Indirect digital imaging consists of scanning traditional images and the storage of phosphor imaging. The components for indirect digital imaging include a CCD camera and a computer. An existing x-ray film is digitized using a CCD camera and the image is displayed on a computer monitor. This concept is similar in theory to scanning an image, such as a photograph, to a computer screen. An image is similar to a “copy” of the image versus the “original.”
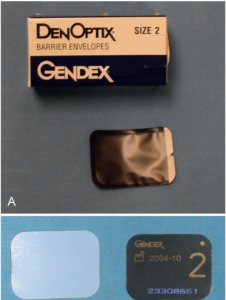
Storage Phosphor Imaging/AKA Photo-Stimulable Phosphor Imaging (PSP)
Photo-stimulable phosphor imaging (PSP) is a wireless digital imaging system. It is a reusable imaging plate coated with phosphors is used instead of a sensor with a fiber optic cable. The phosphor-coated plates are flexible and fit into the mouth and a high-speed scanner is used to convert the information into electronic files. This type of digital imaging is less rapid than direct digital imaging.
Here is an image of a beam alignment device, which holds a PSP digital sensor for a bite-wing image exposure.

Below is an image of a storage phosphor imaging system illustrating the laser scanning device and the intraoral and extraoral PSP digital sensors. A full mouth series of intraoral images is seen on the computer monitor.

Step-by-Step Procedures
It is critical to refer to the manufacturer-provided instruction booklet for information concerning the operation of the system, equipment preparation, patient preparation, and exposure for intraoral sensor preparation and intraoral sensor placement.
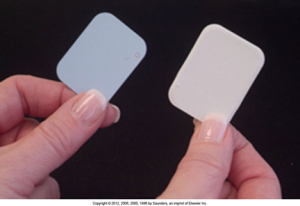
Intraoral Sensor Preparation
For intraoral sensors, each sensor is sealed and waterproofed. The sensor must be covered with a disposable barrier because it cannot be sterilized, and the rigid digital sensors, wired or wireless, must be covered with a disposable barrier sleeve. A rubber finger cot may be placed underneath the disposable barrier sleeve to protect the wired or wireless sensor further and to prevent cross-contamination.
Barrier envelopes are used to seal and protect the PSP sensors from contamination. Below is an example of a PSP sensor, the blue side facing the teeth and the radiation source and the black side facing the tongue.
A wired digital sensor should be wrapped in a protective plastic sleeve so it's ready for intraoral use while maintaining hygiene, which is shown in the image below.

Intraoral Sensor Placement
Intraoral sensor placement is when the sensor is held in the mouth by bite-block attachments or devices that aim the beam and sensor accurately. The paralleling technique is the preferred exposure method. As with conventional intraoral film, the sensor is centered over the area of interest.
Advantages of Digital Imaging
The following are the advantages of digital imaging:
- Superior gray-scale resolution - digital radiography uses up to 256 colors of gray compared with the 16 to 25 shades of gray differentiated on a conventional film.
- Reduced exposure to x-radiation - the exposure of digital radiography is 50% to 90% less than conventional radiography.
- Increased speed of image viewing - instantaneous
- Lower equipment and film cost - no processing equipment or solutions
- Increased efficiency - dental professionals can be more productive
- Enhancement of diagnostic image - the ability to manipulate the density and contrast of the radiographic image without additional exposure to the patient is also an advantage.
- Effective patient education tool
- Eco-friendly tool
Another advantage is that the magnification of a periapical image allows the dental professional to take a closer look at teeth #36 and #37, as shown in the image below.

The advantage of digital subtraction of a bite-wing image is that the grayscale is reversed, eliminating distractions and providing background information.
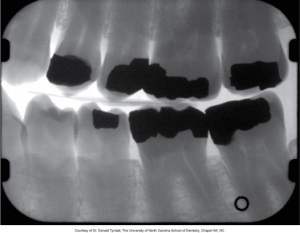
Patient education is also made easier with larger-sized radiographic images.

Disadvantages of Digital Imaging
The following are the disadvantages of digital imaging:
- Initial set-up costs $$$$$
- Image quality - at one time, this was a source of debate. A conventional dental x-ray has a resolution of 12 to 20 lp/mm (line pairs per mm), digital imaging has a resolution of 10 lp/mm, and the human eye can only detect 8-10 lp/mm
- Sensor size - some digital x-ray sensors are thicker and less flexible than intraoral film.
- Infection control - some digital sensors cannot withstand heat sterilization; therefore, sensors require complete coverage with plastic sleeves that must be changed for each patient.
- Wear and tearSensors vulnerable to wear and tear. Handle very carefully! - phosphor plates are not designed to have their edges bent or softened, and if bending or scratching occurs on the plate, permanent defects will appear on ALL the images.
- Legal issues - because the original digital image can be enhanced, it is questionable whether it can be used as evidence in court. Most manufacturers have software with a warning feature that an image has been altered, and the software always keeps a copy of the original.
-
You have completed all of the Module 2 chapters. Please return to Blackboard to complete the Chapter Case Study Quiz.
Media Attributions
- Iannucci & Howerton: Dental Radiography Priniciples and Techniques, 6th Edition, Chapter 8, CC BY-NC-ND

