Total parenteral nutrition (TPN), also known as parenteral nutrition (PN) is a form of nutritional support given completely via the bloodstream, intravenously with an IV pump. TPN administers proteins, carbohydrates, fats, vitamins, and minerals. It aims to prevent and restore nutritional deficits, allowing bowel rest while supplying adequate caloric intake and essential nutrients, and removing antigenic mucosal stimuli (Perry et al., 2014).
TPN may be short-term or long-term nutritional therapy, and may be administered on acute medical floors as well as in critical care areas. The caloric requirements of each patient are individualized according to the degree of stress, organ failure, and percentage of ideal body weight. TPN is used with patients who cannot orally ingest or digest nutrition (Triantafillidis & Papalois, 2014). TPN may be administered as peripheral parenteral nutrition (PPN) or via a central line, depending on the components and osmolality. Central veins are usually the veins of choice because there is less risk of thrombophlebitis and vessel damage (Chowdary & Reddy, 2010). According to Chowdary & Reddy (2010), candidates for TPN are:
-
Patients with paralyzed or nonfunctional GI tract, or conditions that require bowel rest, such as small bowel obstruction, ulcerative colitis, or pancreatitis
-
Patients who have had nothing by mouth (NPO) for seven days or longer
- Critically ill patients
-
Babies with an immature gastrointestinal system or congenital malformations
- Patients with chronic or extreme malnutrition, or chronic diarrhea or vomiting with a need for surgery or chemotherapy
- Patients in hyperbolic states, such as burns, sepsis, or trauma
TPN is made up of two components: amino acid/dextrose solution and a lipid emulsion solution (see Figure 8.9). It is ordered by a physician, in consultation with a dietitian, depending on the patient’s metabolic needs, clinical history, and blood work. The amino acid/dextrose solution is usually in a large volume bag (1,000 to 2,000 ml), and can be standard or custom-made. It is often yellow in colour due to the multivitamins it contains. The ingredients listed on the bag must be confirmed by the health care provider hanging the IV bag. The solution may also include medication, such as insulin and heparin. The amino acid/dextrose solution is reviewed and adjusted each day based on the patient’s blood work. Lipid emulsions are prepared in 100 to 250 ml bags or glass bottles and contain the essential fatty acids that are milky in appearance. At times, the lipid emulsion may be added to the amino acid/dextrose solution. It is then called 3 in 1 or total nutrition admixture (Perry et al., 2014).
TPN is prepared by a pharmacy, where the calories are calculated using a formula, and is usually mixed for a 24-hour continuous infusion to prevent vascular trauma and metabolic instability (North York Hospital, 2013). TPN orders should be reviewed each day, so that changes in electrolytes or the acid-base balance can be addressed appropriately without wasting costly TPN solutions (Chowdary & Reddy, 2010).
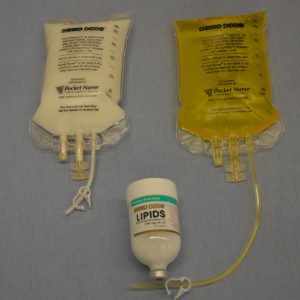

TPN is not compatible with any other type of IV solution or medication and must be administered by itself. TPN must be administered using an EID (IV pump), and requires special IV filter tubing (see Figure 8.10) for the amino acids and lipid emulsion to reduce the risk of particles entering the patient. Agency policy may allow amino acids and lipid emulsions to be infused together above the filters. TPN tubing will not have any access ports and must be changed according to agency policy. Always review agency policy on setup and equipment required to infuse TPN.
A physician may order a total fluid intake (TFI) for the amount of fluid to be infused per hour to prevent fluid overload in patients receiving TPN. It is important to keep track of all the fluids infusing (IV fluids, IV medications, and TPN) in order to avoid fluid overload (Perry et al., 2014). Do not abruptly discontinue TPN (especially in patients who are on insulin) because this may lead to hypoglycemia. If for whatever reason the TPN solution runs out while awaiting another bag, hang D5W at the same rate of infusion while waiting for the new TPN bag to arrive (North York Hospital, 2013). Do not obtain blood samples or central venous pressure readings from the same port as TPN infusions. To prevent severe electrolyte and other metabolic abnormalities, the infusion rate of TPN is increased gradually, starting at a rate of no more than 50% of the energy requirements (Mehanna, Nankivell, Moledina, & Travis, 2009).
Complications Related to TPN
There are many complications related to the administration of TPN (Perry et al., 2014). Table 8.8 lists potential complications, rationale, and interventions.
| Table 8.8 TPN Complications, Rationale, and Interventions | |||
| Complication | Rationale and Interventions | ||
|---|---|---|---|
| Catheter-related bloodstream infection (CR-BSI), also known as sepsis | CR-BSI, which starts at the hub connection, is the spread of bacteria through the bloodstream. There’s an increased risk of CR-BSI with TPN, due to the high dextrose concentration of TPN. Symptoms include tachycardia, hypotension, elevated or decreased temperature, increased breathing, decreased urine output, and disorientation.
Interventions: Strict adherence to aseptic technique with insertion, care, and maintenance; avoid hyperglycemia to prevent infection complications; closely monitor vital signs and temperature. IV antibiotic therapy is required. Monitor white blood cell count and patient for malaise. Replace IV tubing frequently as per agency policy (usually every 24 hours). |
||
| Localized infection at exit or entry site | Due to poor aseptic technique during insertion, care, or maintenance of central line or peripheral line
Interventions: Apply strict aseptic technique during insertion, care, and maintenance. Frequently assess CVC site for redness, tenderness, or drainage. Notify health care provider of any signs and symptoms of infection. |
||
| Pneumothorax | A pneumothorax occurs when the tip of the catheter enters the pleural space during insertion, causing the lung to collapse. Symptoms include sudden chest pain, difficulty breathing, decreased breath sounds, cessation of normal chest movement on affected side, and tachycardia.
Interventions: Apply oxygen, notify physician. Patient will require removal of central line and possible chest tube insertion. |
||
| Air embolism | An air embolism may occur if IV tubing disconnects and is open to air, or if part of catheter system is open or removed without being clamped. Symptoms include sudden respiratory distress, decreased oxygen saturation levels, shortness of breath, coughing, chest pain, and decreased blood pressure.
Interventions: Make sure all connections are clamped and closed. Clamp catheter, position patient in left Trendelenburg position, call health care provider, and administer oxygen as needed. |
||
| Hyperglycemia | Related to sudden increase in glucose after recent malnourished state. After starvation, glucose intake suppresses gluconeogenesis by leading to the release of insulin and the suppression of glycogen. Excessive glucose may lead to hyperglycemia, with osmotic diuresis, dehydration, metabolic acidosis, and ketoacidosis. Excess glucose also leads to lipogenesis (again caused by insulin stimulation). This may cause fatty liver, increased CO2 production, hypercapnea, and respiratory failure.
Interventions: Monitor blood sugar frequently QID (four times per day), then less frequently when blood sugars are stable. Follow agency policy for glucose monitoring with TPN. Be alert to changes in dextrose levels in amino acids and the addition/removal of insulin to TPN solution. |
||
| Refeeding syndrome | Refeeding syndrome is caused by rapid refeeding after a period of malnutrition, which leads to metabolic and hormonal changes characterized by electrolyte shifts (decreased phosphate, magnesium, and potassium in serum levels) that may lead to widespread cellular dysfunction. Phosphorus, potassium, magnesium, glucose, vitamin, sodium, nitrogen, and fluid imbalances can be life-threatening. High-risk patients include the chronically undernourished and those with little intake for more than 10 days. Patients with dysphagia are at higher risk. The syndrome usually occurs 24 to 48 hours after refeeding has started. The shift of water, glucose, potassium, phosphate, and magnesium back into the cells may lead to muscle weakness, respiratory failure, paralysis, coma, cranial nerve palsies, and rebound hypoglycemia.
Interventions: Rate of TPN should be based on the severity of undernourishment for moderate- to high-risk patients. TPN should be initiated slowly and titrated up for four to seven days. All patients require close monitoring of electrolytes (daily for one week, then usually three times/week). Always follow agency policy. Blood work may be more frequent depending on the severity of the malnourishment. |
||
| Fluid excess or pulmonary edema | Signs and symptoms include fine crackles in lower lung fields or throughout lung fields, hypoxia (decreased O2 sats).
Interventions: Notify primary health care provider regarding change in condition. Patient may require IV medication, such as Lasix to remove excess fluids. A decrease or discontinuation of IV fluids may also occur. Raise head of bed to enhance breathing and apply O2 for oxygen saturation less than 92% or as per agency protocol. Monitor intake and output. Pulmonary edema may be more common in the elderly, young, and patients with renal or cardiac conditions. |
||
| Data source: Chowdary & Reddy, 2010; Mehanna et al., 2009; O’Connor, Hanly, Francis, Keane, & McNamara, 2013; Perry et al., 2014 | |||
A patient on TPN must have blood work monitored closely to prevent the complications of refeeding syndrome. Blood work may be ordered as often as every six hours upon initiation of TPN. Most hospitals will have a TPN protocol to follow for blood work. Common blood work includes CBC (complete blood count), electrolytes (with special attention to magnesium, potassium, and phosphate), liver enzymes (total and direct bilirubin, alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase [ALP], gamma-glutamyl transferase [GGT], total protein, albumin), and renal function tests (creatinine and urea). Compare daily values to baseline values, and investigate and report any rapid changes in any values (Chowdary & Reddy, 2010; Perry et al., 2014). Table 8.9 outlines a plan of care when a patient is receiving TPN.
| Table 8.9 Assessment of a Patient with TPN | |||
| Assessment | Additional Information | ||
|---|---|---|---|
| CVC/peripheral IV line | Intravenous line should remain patent, free from infection.
Dextrose in TPN increases risk of infection. Assess for signs and symptoms of infections at site (redness, tenderness, discharge) and systemically (fever, increased WBC, malaise). Dressing should be dry and intact. |
||
| Daily or biweekly weights | Monitor for evidence of edema or fluid overload. Over time, measurements will reflect weight loss/gain from caloric intake or fluid retention. | ||
| Capillary or serum blood glucose levels | QID (4 times a day) capillary blood glucose initially to monitor glycemic control, then reduce monitoring when blood sugars are stable or as per agency policy. May be done more frequently if glycemic control is difficult. Indicates metabolic tolerance to dextrose in TPN solution and patient’s glycemic status. | ||
| Monitor intake and output | Monitor and record every eight hours or as per agency policy. Monitor for signs and symptoms of fluid overload (excessive weight gain) by completing a cardiovascular and respiratory assessment. Assess intakes such as IV (intravenous fluids), PO (oral intake), NG (nasogastric tube feeds). Assess outputs: NG (removed gastric content through the nasogastic tube), fistula drainage, BM (liquid bowel movements), colostomy/ileostomy drainage, closed suction drainage devices (Penrose or Jackson-Pratt drainage) and chest tube drainage. | ||
| Daily to weekly blood work | Review lab values for increases and decreases out of normal range. Lab values include CBC, electrolytes, calcium, magnesium, phosphorus, potassium, glucose, albumin, BUN (blood urea nitrogen), creatinine, triglycerides, and transferrin. | ||
| Mouth care | Most patients will be NPO. Proper oral care is required as per agency policy. Some patients may have a diet order. | ||
| Vital signs | Vital signs are more frequently monitored initially in patients with TPN. | ||
| Data source: BCIT, 2015a; Perry et al., 2014 | |||
TPN may be administered in the hospital or in a home setting. Generally, patients receiving TPN are quite ill and may require a lengthy stay in the hospital. The administration of TPN must follow strict adherence to aseptic technique, and includes being alert for complications, as many of the patients will have altered defence mechanisms and complex conditions (Perry et al., 2014). To administer TPN, follow the steps in Checklist 76.
Checklist 76: TPN AdministrationDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Review physician’s orders and compare to MAR and content label on TPN solution bag and for rate of infusion. Each component of the TPN solution must be verified with the physician’s orders. | Check date and time of last TPN tubing change, lab values, and expiry date of TPN to prevent medication error.
Assess CVC, WBC, and patient for malaise. Medications may be added to the TPN. Ensure the rate of infusion is verified in the doctor’s order each time new TPN bag is initiated. |
||
| 2. Collect supplies, prepare TPN solution, and prime IV tubing with filter as per agency protocol. TPN requires special IV tubing with a filter. | Generally, new TPN tubing is required every 24 hours to prevent catheter-related bacteremia. Follow agency policy.
Ensure tubing is primed correctly to prevent air embolism.  |
||
| 3. Perform hand hygiene, identify yourself, and identify patient using two patient identifiers. Compare the MAR to the patient’s wristband. Explain the procedure to the patient. | Hand hygiene prevents the spread of microorganisms.
Proper identification prevents patient errors. 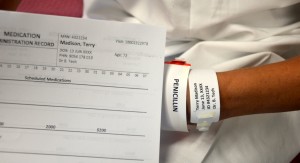 |
||
| 4. Complete all safety checks for CVC as per agency policy. | This adheres to safety policies related to central line care. | ||
| 5. If changing TPN solution, pause EID and remove old TPN administration set. Disinfect connections and change IV tubing as per agency policy.
If starting TPN for the first time, flush and disinfect CVC lumens as per agency policy. |
Change TPN IV tubing as per agency policy. Use strict aseptic technique with IV changes as patients with high dextrose solutions are at greater risk of developing infections. | ||
| 6. Insert new TPN solution and IV tubing into EID. | EID must be used with all TPN administration. | ||
| 7. Start TPN infusion rate as per physician orders. | Prevents medication errors. | ||
| 8. Discard old supplies as per agency protocol, and perform hand hygiene. | These steps prevent the spread of microorganisms. | ||
| 9. Monitor for signs and symptoms of complications related to TPN. | See Table 8.8 for list of complications related to TPN. | ||
| 10. Complete daily assessments and monitoring for patient on TPN as per agency policy. | See daily and weekly assessments in Table 8.9. Flow rate may be monitored hourly. | ||
| 11. Document the procedure in the patient chart as per agency policy. | Note time when TPN bag is hung, number of bags, and rate of infusion, assessment of CVC site and verification of patency, status of dressing, vital signs and weight, client tolerance to TPN, client response to therapy, and understanding of instructions. | ||
| Data source: North York Hospital, 2013; Perry et al., 2014 | |||
Critical Thinking Exercises
- Describe refeeding syndrome and state one method to reduce the risk of refeeding syndrome.
- A patient receiving TPN for the past 48 hours has developed malaise and hypotension. What potential complication are these signs and symptoms related to?

