Drain Management
Drains systems are a common feature of post-operative surgical management and are used to remove drainage from a wound bed to prevent infection and the delay of wound healing. A drain may be superficial to the skin or deep in an organ, duct, or a cavity such as a hematoma. The number of drains depends on the extent and type of surgery. A closed system uses a vacuum system to withdraw fluids and collects the drainage into a reservoir. Closed systems must be emptied and measured at least once every shift and cleaned using sterile technique according to agency protocol.
Drainage tubes consist of silastic tubes with perforations to allow fluid to drain from the surgical wound site, or separate puncture holes close to the surgical area. The drainage is collected in a closed sterile collection system/reservoir (Hemovac or Jackson-Pratt) or an open system that deposits the drainage on a sterile dressing. Drainage may vary depending on location and type of surgery. A Hemovac drain (see Figure 4.3) can hold up to 500 ml of drainage. A Jackson-Pratt (JP) drain (see Figure 4.4) is usually used for smaller amounts of drainage (25 to 50 ml). Drains are usually sutured to the skin to prevent accidental removal. The drainage site is covered with a sterile dressing and should be checked periodically to ensure the drain is functioning effectively and that no leaking is occurring.


Checklist 39 outlines the steps to take when emptying a closed wound drainage system.
Checklist 39: Emptying a Closed Wound Drainage SystemDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Perform hand hygiene. | Hand hygiene reduces the risk of infection. | ||
| 2. Collect the necessary supplies. | For example: drainage measurement container, non-sterile gloves, waterproof pad, and alcohol swab | ||
| 3. Apply non-sterile gloves and goggles or face shield according to agency protocols. | Personal protective equipment reduces the transmission of microorganisms and protects against an accidental body fluid exposure.
 |
||
| 4. Maintaining sterile technique, remove plug from pouring spout as indicated on drain. | Open plug pointing away from your face to avoid an accidental splash of contaminated fluid.
Maintain the plug’s sterility. The vacuum will be broken and the reservoir (drainage collection system) will expand.  |
||
| 5. Gently tilt the opening of the reservoir toward the measuring container and pour out the drainage. | Pour away from yourself to prevent exposure to body fluids. | ||
| 6. Place drainage container on bed or hard surface, tilt away from your face, and compress the drain to flatten it with one hand.
With the other hand, swab the surface of the port, then insert the plug to close the drainage system. |
Gently squeezing the drain to flatten and remove all the air prior to closing the spout will establish the vacuum system.
  |
||
| 7. Place the plug back into the pour spout of the drainage system, maintaining sterility. | This establishes vacuum suction for drainage system.
  |
||
| 8. Secure device onto patient’s gown using a safety pin; check patency and placement of tube.
Ensure that enough slack is present in tubing, and that reservoir hangs lower than the wound. |
Proper placement of the reservoir allows gravity to facilitate wound drainage. Providing enough slack to accommodate patient movement prevents tension of the drainage system and pulling on the tubing and insertion site. | ||
| 9. Note character of drainage: colour, consistency, odour, amount.
Discard drainage according to agency policy. |
Drainage counts as patient fluid output and must be documented on patient chart as per hospital protocol.
Monitor drains frequently in the post-operative period to reduce the weight of the reservoir and to monitor drainage. |
||
| 10. Remove gloves and perform hand hygiene. | Hand hygiene must be performed after removing gloves. Gloves are not puncture-proof or leak-proof, and hands may become contaminated when gloves are removed.
  |
||
|
11. Document procedure and findings according to agency policy. Report any unusual findings or concerns to the appropriate health care professional. |
This allows for an accurate recording of drainage.
Record the number the drains if there is more than one, and record each one separately. If the amount of drainage increases or changes, notify the appropriate health care provider according to agency policy. If amount of drainage significantly decreases, the drain may be ready to be assessed and removed. |
||
| Data source: BCIT, 2010b; Perry et al., 2014 | |||
Drain Removal
Removal of a drain must be ordered by the physician or NP. A drain is usually in place for 24 to 48 hours, and removal depends on the amount of drainage over the last 24 hours.
Checklist 40 outlines the steps for removing a wound drainage system.
Checklist 40: Drain RemovalDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Confirm that the physician order correlates with amount of drainage in the past 24 hours. | Physicians should specify an amount for acceptable drainage for the drain to be removed. | ||
| 2. Explain procedure to patient; offer analgesia and bathroom as required. | Taking this step decrease the patient’s anxiety about the procedure. Explain to the patient that a pulling sensation may be felt but will stop after the procedure is complete.
Analgesia provides comfort and achieves the goal of an acceptable pain level for the procedure. |
||
| 3. Assemble supplies at patient’s bedside: dressing tray, sterile suture scissors or a sterile blade, cleansing solution, extra gauze, tape, garbage bag. | Organizing supplies helps the procedure occur as efficiently as possible for the patient. | ||
| 4. Apply a waterproof drape/pad for depositing the drain once it has been removed. | This provides a place to put the drain once it is removed. | ||
| 5. Perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
| 6. Apply non-sterile gloves and face shield according to agency policy. | Personal protective equipment reduces the potential for accidental exposure to blood or body fluids.
 |
||
| 7. Release suction on reservoir and empty; measure and record drainage if >10 ml. | Releasing suction reduces potential for tissue damage as drain is removed.
 |
||
| 8. Remove tape and dressing from drain insertion site. | Remove tape to allow for ease of drain removal. | ||
| 9. Cleanse site according to simple dressing change procedure. | This step prevents infection of the site and allows the suture to be easily seen for removal.
 |
||
| 10. Carefully cut and remove suture anchoring drain with sterile suture scissors or a sterile blade. |
 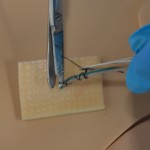 Snip beneath the suture knot to ensure contaminated suture is not brought into the tissue. Pull suture out. Snip or cut knot away from yourself. |
||
| 11. Stabilize skin with non-dominant hand. | Applying counterpressure to skin near the drain decreases discomfort to patient. | ||
| 12. Ask patient to take a deep breath and exhale slowly; remove the drain as the patient exhales. | This step helps the patient prepare for removal of the drain. | ||
| 13. Firmly grasp drainage tube close to skin with dominant hand, and with a swift and steady motion withdraw the drain and place it on the waterproof drape/pad (other hand should stabilize skin with 4 x 4 sterile gauze around drain site). | Slight resistance may be felt.
If there is strong resistance, stop, cover site, and call physician. Ensure the drainage tip is intact. The end of the drainage tip should be smooth. Some agencies require that the tip be sent for lab analysis for microorganisms. When pulling out drain, gather up the drain tubing in your hand as it’s being removed. 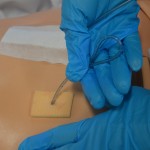 |
||
| 14. Place drain and tube on waterproof pad or in garbage bag to be disposed of after procedure is complete. | This step prevents the drain and tube from contaminating bed or floor. | ||
| 15. Remove gloves and apply new non-sterile gloves. | This prevents contamination of the drain site.
  |
||
| 16. Cleanse old drain site using aseptic technique according to simple dressing change procedure. | This step prevents contamination of the drain site. | ||
| 17. Cover drain site with sterile dressing. |
 |
||
| 18 Assist patient back to comfortable position and lower bed. | This ensures patient safety and comfort after the procedure. | ||
| 19. Discard drain in biohazard waste as per hospital policy. | This prevents the spread of microorganisms. | ||
| 20. Perform hand hygiene. | Hand hygiene prevents the spread of infection.
 |
||
| 21. Document output and drain removal. | Record drainage according to agency policy. | ||
| 22. Assess dressing 30 minutes after drain removal. | Monitor for excessive drainage from the drainage site.
 |
||
| 23. Document procedure and findings according to agency policy.
Report any unusual findings or concerns to the appropriate health care professional. |
Accurate and timely documentation and reporting promote patient safety. | ||
| Data source: BCIT, 2010b; Perry et al., 2014; Saskatoon Health Region, 2012 | |||
Critical Thinking Exercises
- When you start to remove your patient’s Jackson-Pratt drain, you notice there is 100 ml of fresh blood in the drainage bulb. What would be your next steps?
- Describe ways in which you can help relieve the discomfort felt by a patient while removing a wound drain.


