Sutures are tiny threads, wire, or other material used to sew body tissue and skin together. They may be placed deep in the tissue and/or superficially to close a wound. A variety of suture techniques are used to close a wound, and deciding on a specific technique depends on the location of the wound, thickness of the skin, degree of tensions, and desired cosmetic effect (Perry et al., 2014).
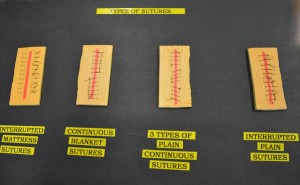
There are three types of sutures techniques: intermittent, blanket, and continuous (see Figure 4.2). The most commonly seen suture is the intermittent suture.
Sutures may be absorbent (dissolvable) or non-absorbent (must be removed). Non-absorbent sutures are usually removed within 7 to 14 days. Suture removal is determined by how well the wound has healed and the extent of the surgery. Sutures must be left in place long enough to establish wound closure with enough strength to support internal tissues and organs.
The health care provider must assess the wound to determine whether or not to remove the sutures. The wound line must also be observed for separations during the process of suture removal. Removal of sutures must be ordered by the primary health care provider (physician or nurse practitioner). An order to remove sutures must be obtained prior to the procedure, and a comprehensive assessment of the wound site must be performed prior to the removal of the sutures by the health care provider.
Alternate sutures (every second suture) are typically removed first, and the remaining sutures are removed once adequate approximation of the skin tissue is determined. If the wound is well healed, all the sutures would be removed at the same time. Alternately, the removal of the remaining sutures may be days or weeks later (Perry et al., 2014). Checklist 34 provides the steps for intermittent suture removal.
Checklist 34: Intermittent Suture RemovalDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Confirm physician/nurse practitioner (NP) orders, and explain procedure to patient. | Explaining the procedure will help prevent anxiety and increase compliance with the procedure.
Inform patient that the procedure is not painful but the patent may feel some pulling of the skin during suture removal. |
||
| 2. Gather appropriate supplies. | You will need sterile suture scissors or suture blade, sterile dressing tray (to clean incision site prior to suture removal), non-sterile gloves, normal saline, Steri-Strips, and sterile outer dressing. | ||
| 3. Position patient appropriately and create privacy for procedure. | Ensure proper body mechanics for yourself and create a comfortable position for the patient. | ||
| 4. Perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
| 5. Prepare the sterile field and add necessary supplies in an organized manner. | This allows easy access to required supplies for the procedure.
 |
||
| 6. Remove dressing and inspect the wound using non-sterile gloves. | Visually assess the wound for uniform closure of the wound edges, absence of drainage, redness, and swelling.
Pain should be minimal. After assessing the wound, decide if the wound is sufficiently healed to have the sutures removed. If there are concerns, question the order and seek advice from the appropriate health care provider.  |
||
| 7. Remove non-sterile gloves and perform hand hygiene. | This prevents the transmission of microorganisms.
 |
||
| 8. Apply clean non-sterile gloves. | This prevents the transmission of microorganisms.
 |
||
| 9. Clean incision site according to agency policy. | This step reduces risk of infection from microorganisms on the wound site or surrounding skin.
 Cleaning also loosens and removes any dried blood or crusted exudate from the sutures and wound bed. |
||
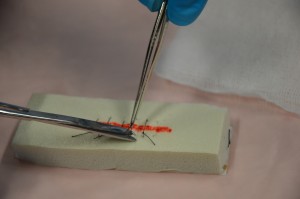
| 10. To remove intermittent sutures, hold scissors in dominant hand and forceps in non-dominant hand. | This allows for dexterity with suture removal.
 |
||
| 11. Place a sterile 2 x 2 gauze close to the incision site. | The sterile 2 x 2 gauze is a place to collect the removed suture pieces.
 |
||
| 12. Grasp knot of suture with forceps and gently pull up knot while slipping the tip of the scissors under suture near the skin. Examine the knot. |
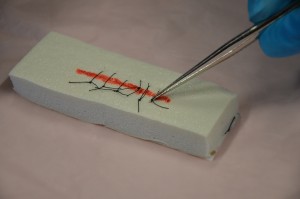 |
||
| 13. Cut under the knot as close as possible to the skin at the distal end of the knot.
|
 Never snip both ends of the knot as there will be no way to remove the suture from below the surface. Do not pull the contaminated suture (suture on top of the skin) through tissue. If using a blade to cut the suture, point the blade away from you and your patient. |
||
| 14. Grasp knotted end with forceps, and in one continuous action pull suture out of the tissue and place cut knot on sterile 2 x 2 gauze. |
 |
||
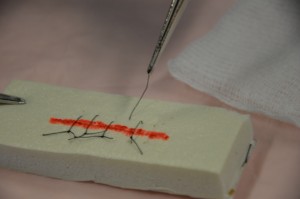
| 15. Remove every second suture until the end of the incision line. | Assess wound healing after removal of each suture to determine if each remaining suture will be removed. | ||
| If wound edges open, stop removing sutures, apply Steri-Strips (using tensions to pull wound edges together), and notify appropriate health care providers. | |||
| 16. Using the principles of sterile technique, place Steri-Strips on location of every removed suture along incision line. |
 |
||
| 17. Cut Steri-Strips so that they extend 1.5 to 2 inches on each side of incision. | Steri-Strips support wound tension across wound and help to eliminate scarring.
 |
||
| 18. Remove remaining sutures on incision line if indicated.
|
Only remove remaining sutures if wound is well approximated.
 |
||
| 19. Place Steri-Strips on remaining areas of each removed suture along incision line. | The Steri-Strips will help keep the skin edges together.
 |
||
| Data source: BCIT, 2010c; Perry et al., 2014 | |||
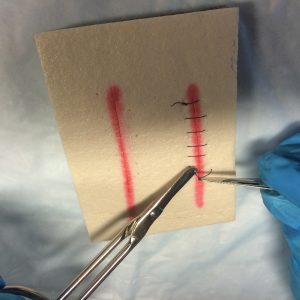
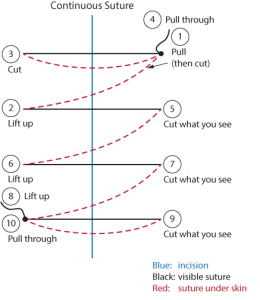
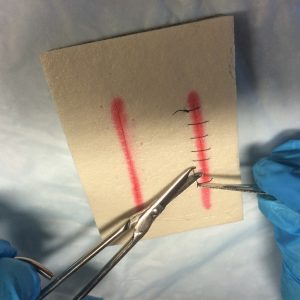
Checklist 35 outlines the steps to remove continuous and blanket stitch sutures.
Checklist 35: Continuous and Blanket Stitch Suture RemovalDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Confirm physician/NP orders, and explain procedure to patient. | Explaining the procedure will help prevent anxiety and increase compliance with the procedure.
Inform patient that the procedure is not painful but the patent may feel some pulling of the skin during suture removal. |
||
| 2. Gather appropriate supplies. | You will need sterile suture scissors or suture blade, sterile dressing tray (to clean incision site prior to suture removal), non-sterile gloves, normal saline, Steri-Strips, and sterile outer dressing. | ||
| 3. Position patient appropriately and create privacy for procedure. | Ensure proper body mechanics for yourself and create a comfortable position for the patient. | ||
| 4. Perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
| 5. Prepare the sterile field and add necessary supplies in an organized manner. | This step allows for easy access to required supplies for the procedure.
 |
||
| 6. Remove dressing and inspect the wound using non-sterile gloves. | Visually assess the wound for uniform closure of the wound edges, absence of drainage, redness, and swelling.
Pain should be minimal.  After assessing the wound, decide if the wound is sufficiently healed to have the sutures removed. If there are concerns, question the order and seek advice from the appropriate health care provider. |
||
| 7. Remove non-sterile gloves and perform hand hygiene. | This step prevents the transmission of microorganisms.
 |
||
| 8. Apply clean non-sterile gloves. | This prevents the transmission of microorganisms.
 |
||
| 9. Clean incision site according to agency policy. | This step reduces the risk of infection from microorganisms on the wound site or surrounding skin.
Cleaning also loosens and removes any dried blood or crusted exudate from the sutures and wound bed.  |
||
| 10. Place sterile gauze close to suture line; grasp scissors in dominant hand and forceps in non-dominant hand. | This allows for dexterity with suture removal. | ||
| 11. Snip first suture close to the skin surface, distal to the knot. |
 |
||
| 12. Snip second suture on the same side. | This action prevents the suture from being left under the skin. | ||
| 13. Grasp knotted end and gently pull out suture; place suture on sterile gauze. |
 |
||
| 14. Continue cutting in the same manner until the entire suture is removed, inspecting the incision line during the procedure. | Inspection of incision line reduces the risk of separation of incision during procedure. | ||
| If separation occurs, stop procedure, apply Steri-Strips, and notify physician. | |||
| 15. Apply Steri-Strips to suture line, then apply sterile dressing or leave open to air. | This step reduces the risk of infection.
 |
||
| 16. Position patient and lower bed to safe height; ensure patient is comfortable and free from pain. | This ensures patient safety. | ||
| 17. Complete patient teaching regarding Steri-Strips and bathing, wound inspection for separation of wound edges, and ways to enhance wound healing. | Instruct patient to take showers rather than bathe.
Instruct patient to pat dry, and to not scrub or rub the incision. Instruct patient not to pull off Steri-Strips. Allow the Steri-Strips to fall off naturally and gradually (usually takes one to three weeks). Instruct patient about the importance of not straining during defecation, and the importance of adequate rest, fluids, nutrition, and ambulation for optional wound healing. |
||
| 18. Discard supplies according to agency policies for sharp disposal and biohazard waste. | Scissors and forceps may be disposed of or sent for sterilization. | ||
| 19. Perform hand hygiene. | Hand hygiene reduces risk of infection.
 |
||
| 20. Document procedures and findings according to agency policy. | Report any unusual findings or concerns to the appropriate health care professional. | ||
| Data source: BCIT, 2010c; Perry et al., 2014 | |||
Complications related to suture removal, including wound dehiscence, may occur if wound is not well healed, if the sutures are removed too early, or if excessive force (pressure) is applied to the wound. In addition, if the sutures are left in for an extended period of time, the wound may heal around the sutures, making extraction of the sutures difficult and painful. Table 4.4. lists additional complications related to wounds closed with sutures.
| Table 4.4 Complications of Suture Removal | |||
| Complication | Solution | ||
|---|---|---|---|
| Unable to remove suture from tissue | Contact physician for further instructions. | ||
| Wound dehiscence: Incision edges separate during suture removal; wound opens up | Stop removing sutures.
Apply Steri-Strips across open area. Notify physician. |
||
| Patient experiences pain when sutures are removed | Allow small breaks during removal of sutures.
Provide opportunity for the patient to deep breathe and relax during the procedure. |
||
| Wound becomes red, painful, with increasing pain, fever, drainage from wound | These changes may indicate the wound is infected. Report findings to the primary health care provider for additional treatment and assessments. | ||
| Scarring related to sutures | All wounds form a scar and will take months to one year to completely heal. Scarring may be more prominent if sutures are left in too long. | ||
| Keloid formation | A keloid formation is a firm scar-like mass of tissue that occurs at the wound site. The scarring tends to extend past the wound and is darker in appearance. | ||
| Hypertrophic scars | Hypertrophic scars are scars that are bulky but remain within the boundaries of the wound. These scars can be minimized by applying firm pressure to the wound during the healing process using sterile Steri-Strips or a dry sterile bandage. | ||
| Data source: BCIT, 2010c; Perry et al., 2014 | |||
Critical Thinking Exercises
- What is the purpose of applying Steri-Strips to the incision after removing sutures?
- Which health care provider is responsible for assessing the wound prior to removing sutures?

