A chest tube, also known as a thoracic catheter, is a sterile tube with a number of drainage holes that is inserted into the pleural space. The pleural space is the space between the parietal and visceral pleura, and is also known as the pleural cavity. A patient may require a chest drainage system any time the negative pressure in the pleural cavity is disrupted, resulting in respiratory distress. Negative pressure is disrupted when air, or fluid and air, enters the pleural space and separates the visceral pleura from the parietal pleura, preventing the lung from collapsing and compressing at the end of exhalation. A small amount of fluid or air may be absorbed by the body without a chest tube. A large amount of fluid or air cannot be absorbed by the body and will require a drainage system (Bauman & Handley, 2011; Perry et al., 2014).
The chest tube is connected to a closed chest drainage system, which allows for air or fluid to be drained, and prevents air or fluid from entering the pleural space. The system is airtight to prevent the inflow of atmospheric pressure. Because the pleural cavity normally has negative pressure, which allows for lung expansion, any tube connected to it must be sealed so that air or liquid cannot enter the space where the tube is inserted (Bauman & Handley, 2011; Rajan, 2013).
The location of the chest tube depends on what is being drained from the pleural cavity. If air is in the pleural space, the chest tube will be inserted above the second intercostal space at the mid-clavical line. If there is fluid in the pleural space, the chest tube is inserted at the fourth to fifth intercostal space, at the mid-axillary line. A chest tube may also be inserted to drain the pericardial sac after open heart surgery, and may be placed directly under the sternum (Perry et al., 2014).
The following are some of the conditions that may require a chest tube drainage system (Bauman & Handley, 2011; Perry et al., 2014):
- Pleural effusion
- Pneumothorax
- Hemothorax
- Spontaneous pneumothorax
- Tension pneumothorax
- Traumatic pneumothorax (stab or gunshot wound)
- Cardiac tamponade (accumulation of blood surrounding the heart after open heart surgery or chest surgery)
A chest tube drainage system must always be placed below the drainage site and secured in an upright position (attached to the floor or an IV pole, as in Figure 10.4) to prevent it from being knocked over.

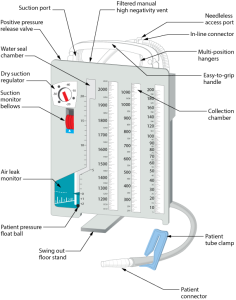
A chest tube drainage system is a sterile, disposable system that consists of a compartment system that has a one-way valve, with one or multiple chambers, to remove air or fluid and prevent return of the air or fluid back into the patient (see Figures 10.5 and 10.6). The traditional chest drainage system typically has three chambers (Bauman & Handley, 2011; Rajan, 2013). Always review what type of system is used in your agency, and follow the agency’s and the manufacturer’s directions for setup, monitoring, and use. In general, a traditional chest tube drainage system will have these three chambers:
- Collection chamber: The chest tube connects directly to the collection chamber, which collects drainage from the pleural cavity. The chamber is calibrated to measure the drainage. The outer surface of the chamber has a “write-on” surface to document the date, time, and amount of fluid. This chamber is typically on the far right side of the system (Teleflex Medical Incorporated, 2009).
- Water-seal chamber: This chamber has a one-way valve that allows air to exit the pleural cavity during exhalation but does not allow it to re-enter during inhalation due to the pressure in the chamber. The water-seal chamber must be filled with sterile water and maintained at the 2 cm mark to ensure proper operation, and should be checked regularly. Fill with additional sterile water as required. The water in the water-seal chamber should rise with inhalation and fall with exhalation (this is called tidaling), which demonstrates that the chest tube is patent. Continuous bubbling may indicate an air leak, and newer systems have a measurement system for leaks — the higher the number, the greater the air leak. The water-seal chamber can also monitor intrathoracic pressure (Teleflex Medical Incorporated, 2009).
- Wet or dry suction control chamber: Not all patients require suction. If a patient is ordered suction, a wet suction system is typically controlled by the level of water in the suction control chamber and is typically set at -20 cm on the suction control chamber for adults. If there is less water, there is less suction. The amount of suction may vary depending on the patient and is controlled by the chest drainage system, not the suction source. Monitor the fluid level to ensure there is gentle bubbling in the chamber. A dry suction system uses a self-controlled regulator that adjusts the amount of suction and responds to air leaks to deliver consistent suction for the patient. If suction is discontinued, the suction port on the chest drainage system must remain unobstructed and open to air to allow air to exit and minimize the development of a tension pneumothorax (Teleflex Medical Incorporated, 2009).
In addition to the three chambers, the drainage system has many safety features to ensure that high negative pressures can be monitored and relieved quickly. To review these safety features and additional information regarding the chambers of a closed chest tube drainage system, visit the Teleflex Medical Incorporated website.
When a patient has a closed chest tube drainage system, it is the health care provider’s responsibility to assess the patient and the equipment frequently to ensure the equipment is patent and working effectively. The health care provider should:
- Assess the patient
- Assess the chest tube drainage system for patency and troubleshoot any concerns
- Ensure the safety/emergency equipment is attached to the bed
- Promote lung expansion (deep breathing and coughing exercises, position changes, and ambulation as required)
Checklist 86 reviews the management of a patient with a chest tube drainage system.
Checklist 86: Management of a Chest Tube Drainage System (Pleur-evac)Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Review the patient chart for the reason for the chest tube and location and insertion date. | Knowing the reason for the chest tube and location informs the health care provider on the type of expected drainage. | ||
| 2. Perform hand hygiene. identify patient using two identifiers and explain assessment process to patient. Create privacy to assess the patient and drainage system. | Hand hygiene reduces the transmission of microorganisms.
Proper identification provides patient safety measures for safe care. |
||
| 3. Complete respiratory assessment, ensure patient has minimal pain, and measure vital signs. Place patient in semi-Fowler’s position for easier breathing. | Patient should be in a semi-Fowler’s position, have minimal pain, have no respiratory distress, and have no evidence of an air leak around the insertion site, and no drainage from the insertion site or chest tube equipment.
Frequent assessment of the respiratory status is important if the patient’s condition is stable, resolving, or worsening, and ensures that the chest tube is functioning correctly. Assessment should be every 15 minutes to 1 hour until patient is stable. Increase monitoring if patient’s condition worsens. Chest tubes are painful, as the parietal pleura are very sensitive. Ensure patient has adequate pain relief, especially prior to repositioning, sitting, or ambulation. |
||
| 4. Assess chest tube insertion site to ensure sterile dressing is dry and intact.
Check insertion site for subcutaneous emphysema. |
Dressing should remain dry and intact; no drainage holes should be visible in the chest tube.
Dressing is generally changed 24 hours post-insertion, then every 48 hours. Chest tubes are generally sutured in place. There should be no fluid leaking from around the site or sounds of air leaks from insertion site.  |
||
| 5. Maintain a closed system. Ensure all connections are taped and secured according to agency policy. | These measures are important to keep the system intact and prevent accidental tube removal or disruption of the drainage system. | ||
| 6. Ensure tubing is not kinked or bent under the patient or in the bed rails, or compressed by the bed. | Kinked or bent tubing could interfere with the drainage of the pleural fluid.
Dependent loops may collect fluid and impede drainage. The long tube may be coiled and secured to a draw sheet with a safety pin (allowing enough tubing so that the patient can move in bed comfortably) to prevent dependent loops.  |
||
| 7. Collection chamber (drainage system) is below the level of the chest and secured to prevent it from being accidentally knocked over. | The drainage system must remain upright for the water-seal chamber to function correctly.
The chest drainage system must be lower than the chest to facilitate drainage and prevent back flow.  |
||
| 8. Periodically check water-seal chamber to ensure water level is to the dotted line (2 cm) — at least once every shift. Add water as necessary. | Adequate water in the water-seal chamber prevents excess suction being placed on the delicate tissue.
Water levels should be checked each shift as the water may evaporate. |
||
| 9. Check water-seal chamber for tidaling (water moving up and down) with respirations. Gentle bubbling is normal as the lungs expand. | If the water in the water seal does not move up and down with respirations, the system might not be intact or patent. Periodic bubbling in the water-seal chamber is normal and indicates that air that is trapped is being removed. Frequent assessment of the system is required to ensure proper functioning.
 Excessive bubbling may cause unnecessary noise and faster evaporation. If there is no tidaling, consider 1) an occlusion somewhere between the pleural cavity and the water seal, or 2) a full expansion of the lung, where suction has drawn the lung up against the holes in the chest tubes. If patient is on positive pressure ventilation, the tidaling will be the opposite: the water will move down with inspiration and up with expiration. |
||
| 10. Ensure suction control dial is set to ordered level (usually 20 cm). | The amount of suction in the chamber is regulated by the suction control dial, not the suction source. | ||
| 11. If suction is ordered, a “float” (or equivalent) must be visible clearly in the window. | In wet suction control, gentle bubbling is normal. If there is no bubbling, ensure the connections are tight and turn the suction higher.
 |
||
| 12. If suction is not ordered, ensure the suction port is left open to air. Suction window will appear blank if suction is not in use or not working. | The suction port must be left open to the air and free of obstruction to prevent a tension pneumonthorax.
  |
||
| 13. In wet suction systems, expect gentle bubbling in the chamber. | Gentle bubbling is normal. Vigorous bubbling is noisy and can be disturbing to the patient. Periodically check the air vent to ensure it is not blocked or occluded. | ||
| 14. Assess air leak meter to determine progress of patient’s internal air level, measured as level 1 to 7. On every shift, document the level of air leak, and if the air leak occurs at rest or with coughing. | Bubbling in the air leak meter indicates an air leak. Measure and monitor.
The source of the leak may be identified by:
Notify doctor of any new, increased, or unexpected air leaks that are not corrected by the above actions. To document the air leak, note the numbered column through which the bubbling occurs. If bubbling is present in first three columns of the air leak meter, document “air leak 3.” 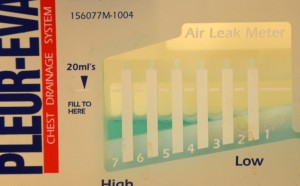 |
||
| 15. Check that the clamp is open. | The chest tube should not be clamped unless for specific reasons. See special considerations below.
 |
||
| 16. Measure date and time, and the amount of drainage, and mark on the outside of the chamber. Record amount and characteristics of the drainage on the fluid balance sheet and patient chart. | Drainage that is red and free-flowing indicates a hemorrhage. A large amount of drainage, or drainage that changes in colour, should be recorded and reported to the primary health care provider.
Drainage that suddenly decreases may indicate a blood clot or obstruction in the chest tube drainage system.  |
||
| 17. Encourage frequent position changes as well as deep-breathing and coughing exercises. | Deep-breathing and coughing exercises promote lung expansion and promote fluid drainage. | ||
18. The following should be documented and assessed according to agency policy:
|
Proper documentation is required to manage a chest tube drainage system to ensure it is functioning effectively. | ||
| Data source: Bauman & Handley, 2011; BCIT, 2015c; Durai, Hoque, & Davies, 2010; Rajan, 2013; Teleflex Medical Incorporated, 2009 | |||
Special considerations:
- Do not strip or milk the chest tube: In practice, stripping is used to describe compressing the chest tube with the thumb or forefinger and, with the other hand, using a pulling motion down the remainder of the tube away from the insertion site. Milking refers to techniques such as squeezing, kneading, or twisting the tube to create bursts of suction to move clots. Any aggressive manipulation (compressing the tube to dislodge blood clots) can generate extreme pressures in the chest tube. There is no evidence showing the benefit of stripping or milking a chest tube (Bauman & Handley, 2011; Durai et al., 2010; Halm, 2007).
- The only exceptions to clamping a chest tube are 1) if the drainage system is being changed, 2) if assessing the system for an air leak, 3) if the chest tube becomes disconnected from the chest drainage system — the chest tube should not be clamped for more than a few minutes (Salmon, Lynch, & Muck, 2013), or 4) if the condition of the patient is resolved and the chest tube is ready for removal (as per physician orders).
Table 10.3 provides a list of potential complications and interventions related to chest tube drainage systems.
| Table 10.3 Complications and Interventions Related to Chest Tube Drainage Systems | |||
| Complications | Interventions | ||
|---|---|---|---|
| Potential pneumothorax/respiratory distress | This is the primary concern for a patient with a chest tube drainage system.
|
||
| Air leak | An air leak may occur from the chest tube insertion site or the drainage system. Do the following to test the system for the site of an air leak:
|
||
| Accidental chest tube removal or chest tube falls out | A chest tube falling out is an emergency. Immediately apply pressure to chest tube insertion site and apply sterile gauze or place a sterile Jelonet gauze and dry dressing over insertion site and ensure tight seal. Apply dressing when patient exhales. If patient goes into respiratory distress, call a code. Notify primary health care provider to reinsert new chest tube drainage system. | ||
| Accidental disconnection of the drainage system | A chest tube drainage system disconnecting from the chest tube inside the patient is an emergency. Immediately clamp the tube and place the end of chest tube in sterile water or NS. The two ends will need to be swabbed with alcohol and reconnected. | ||
| Bleeding at the insertion site | Bleeding may occur after insertion of the chest tube. Apply pressure to site and monitor. | ||
| Subcutaneous emphysema | Subcutaneous emphysema is painless tracking of air underneath the subcutaneous tissue. It may be seen in the chest wall, down limbs, around drain sites, or around the head or neck. When the skin is palpated, it feels similar to having tissue paper trapped beneath the skin. Monitor and report to primary health care provider. | ||
| Drainage suddenly stops and respiratory distress increases | The chest tube may be clogged by a blood clot or by fluid in a dependent loop.
Assess the drainage system and the patient and notify primary health care provider if required. |
||
| Sudden increase in bright red drainage | This may indicate an active bleed. Monitor amount of drainage and vital signs, and notify the primary health care provider. | ||
| Data source: ATI, 2015c; BCIT, 2015c; Perry et al., 2014; Teleflex Medical Incorporated, 2009 | |||
Heimlich Valve
A Heimlich valve (see Figures 10.7 and 10.8) is a small, specially designed flutter valve that is portable and mobile, allowing the patient to ambulate with ease. It attaches to the chest tube at one end and a drainage bag at the other. The drainage bag allows air and fluid to escape but prevents their re-entering the pleural space. The valve can be worn under clothing. The valve functions in any position, never needs to be clamped, and can be hooked up to suction if required (Gogakos et al., 2015).


Critical Thinking Exercises
- What should you do if your patient’s chest tube becomes disconnected from the chest tube drainage system?
- When a patient has a chest tube, what emergency supplies must be at the patient’s bedside at all times?

