Intravenous (IV) is a method of administering concentrated medications (diluted or undiluted) directly into the vein using a syringe through a needleless port on an existing IV line or a saline lock. The direct IV route usually administers a small volume of fluid/medicine (max 20 ml) that is pushed manually into the patient. Medications given by IV are usually administered intermittently to treat emergent concerns. Medications administered by direct IV route are given very slowly over AT LEAST 1 minute (Perry et al., 2014). Administering a medication intravenously eliminates the process of drug absorption and breakdown by directly depositing it into the blood. This results in the immediate elevation of serum levels and high concentration in vital organs, such as the heart, brain, and kidneys. Both therapeutic and adverse effects can occur quickly with direct intravenous administration (Alberta Health Services, 2009).
In the past, IV medications have been called IV bolus or IV push medications. It is recommended that these terms NOT be used, as they can be mistakenly interpreted as meaning the drugs are to be pushed quickly, in less than a minute (ISMP, 2003). To administer IV medications safely and effectively, all health care agencies have policies in place and the Parenteral Drug Therapy Manual (PDTM) that identifies medications that may be given intravenously. (The PDTM may also be referred to as a parenteral drug monograph [Alberta Health Services, 2009].) Only specific medications may be administered via the direct IV route. There are many advantages and disadvantages to administering medications via the intravenous injection method — see Table 7.8.
| Table 7.8 Advantages and Disadvantages of Intravenous Medications | |||
| Advantages | Disadvantages | ||
|---|---|---|---|
| Intravenous medications can deliver an immediate, fast-acting therapeutic effect, which is important in emergent situations such as cardiac arrest or narcotic overdose. They are useful to manage pain and nausea by quickly achieving therapeutic levels, and they are more consistently and completely absorbed compared with medications given by other routes of injection. | Once an intravenous medication is delivered, it cannot be retrieved. When giving IV medications, there is very little opportunity to stop an injection if an adverse reaction or error occurs. IV medications, if given too quickly or incorrectly, can cause significant harm or death. | ||
| Doses of short-acting medication can be titrated according to patient responses to drug therapy. Medication can be prepared quickly and given over a shorter period of time compared to the IV piggyback route. | Any toxic or adverse reaction will occur immediately and may be exacerbated by a rapidly injected medication. | ||
| Minimal dilution is required for some medications, which is desirable for patient’s own fluid restrictions. | Extravasation of certain medications into surrounding tissues can cause sloughing, nerve damage, and scarring. | ||
| There is minimal or no discomfort for the patient in comparison to SC and IM injections. | Not all medications can be given via the direct IV route. | ||
| They provide an alternative to the oral route for drugs that may not be absorbed by the GI tract, and they are ideal for patients with GI dysfunction or malabsorption, and patients who are NPO (nothing by mouth) or unconscious. | There is a high risk for infusion reactions, mild to severe, because most IV medications peak rapidly (i.e., they have a quick onset of effect). A hypersensitivity reaction can occur immediately or be delayed, and requires supportive measures. | ||
| IV direct route provides a more accurate dose of medication because none is left in the intravenous tubing. | Route for administering medications may damage surrounding tissues. There is an increased risk of phlebitis with highly concentrated medication, especially with small peripheral veins or a short venous access device. | ||
| Data source: Albert Health Services, 2009; Lynn, 2011; Perry et al., 2014 | |||
Intravenous medications are always prepared using the SEVEN rights x 3 as per agency policy. Because of the high risk associated with direct intravenous medications, additional guidelines are required. A PDTM or drug monograph provides additional information, which includes the generic name, brand name, classification of the drug, and chart defining which parenteral route may be utilized. Some medications may only be given via a piggyback method or large-volume IV solutions; some medications may be given diluted over 1 or 2 minutes. In addition, information regarding indications, contraindications, dosage (age dependent), administration/dilution guidelines, adverse effects, clinical indications (e.g., specialized monitoring required, must be on an IV pump), compatibility, and incompatibility in relation to reconstitution and primary IV solution is specified (Alberta Health Services, 2009).
The Institute for Safe Medication Practices (ISMP) (2014) has created a list of high-alert medications that bear the heightened risk of significant harm when they are used in error. Special safeguards for these medications can be found in the PDTM. It is vital to understand which medications are considered high risk prior to administration. A link to the list of high-risk medications can be found under Suggested Online Resources at the end of this chapter. Review the steps shown in Table 7.9 to prepare a medication by direct IV route. The PDTM must be consulted every time an IV medication is given, as memory-based errors are common (World Health Organization, 2012).
Before giving an intravenous medication, always assess the IV needle insertion site for signs of infiltration or phlebitis. Start a new IV site if current site is red, swollen, or painful when flushing. Intravenous medications by direct IV route can be given three ways:
- Through a saline lock (short venous access device)
- Through an existing IV line with compatible IV solution
- Through an existing IV with an incompatible IV solution
Checklist 60 reviews the steps to administer an IV medication through a saline lock. Review the preparation questions for intravenous medication in Table 7.9 prior to administering medication.
Checklist 60: Administering an IV Medication via a Saline LockDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety Considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Prepare one medication for one patient at the correct time as per agency policy. Review the physician’s order, PDTM, and MAR for the correct order and guidelines. Math calculations may be required to determine the correct dose to prepare the medication. | Always apply the SEVEN rights x 3 of medication administration.
Review the agency policy if a medication is a stat, given for the first time, a loading dose, or a one-time dose. Some agencies require that high-alert medications be double-checked by a second health care provider. Always follow agency policies. For a list of high-alert medications, see Suggested Online Resources. After preparing the medication, always label the medication syringe with the patient name, date, time, medication, and concentration of the dose (e.g., morphine 2 mg/ml), dose, and your initials. Never leave the medication syringe unattended. |
||
| 2. Create privacy if possible. | This provides comfort to patient. | ||
| 3. Confirm patient ID using two patient identifiers (e.g., name and date of birth) AND compare the MAR printout with the patient’s wristband to confirm patient ID. | This ensures you have the correct patient and complies with agency standard for patient identification.
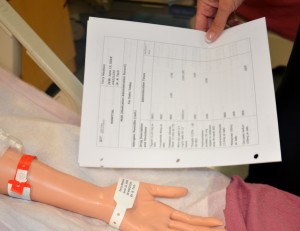 |
||
| 4. Check allergy band for any allergies, and ask patient about type and severity of reaction. | This ensures allergy status is correct on the MAR and on patient allergy band. | ||
| 5. Discuss purpose, action, and possible side effects of the medication. Provide patient an opportunity to ask questions. Encourage patient to report discomfort at the IV site (pain, swelling, or burning). | Keeping patient informed of what is being administered helps decrease anxiety. | ||
| 6. Perform hand hygiene and put on non-sterile gloves. | Hand hygiene prevents the transmission of microorganisms.
 |
||
| 7. Clean access port in a circular motion with an alcohol swab for 15 seconds. Allow to dry. | This technique prevents introduction of microorganisms by the syringe.
 |
||
| 8. Remove air from prefilled syringe. Release clamp on extension tubing and flush the saline lock with 3 to 5 ml of normal saline to ensure patency. Do not force if resistance is felt. Remove syringe. | If swelling, pain, or redness exists, remove IV cannula and restart new IV site. Tenderness is the first sign of phlebitis.
  |
||
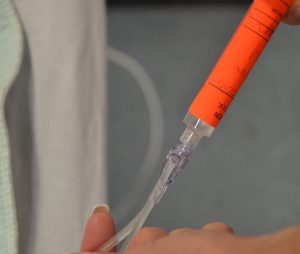
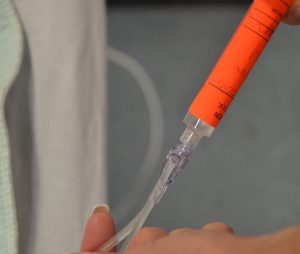
| 9. Attach medication syringe (without needle) to access device. | Using a needleless system prevents needle-stick injuries.
 |
||
| 10. Using a timer with a second hand, inject medication at the correct rate according to agency policy. Use a push-pause method to inject the medication. | Using a timer ensures safe medication administration. Rapid injection of IV medications can be fatal. A slow rate allows medications to be administered correctly.
 |
||
| 11. Remove used medication syringe. Remove air from prefilled NS syringe and attach to the Max Plus device.
Flush (3 to 5 ml) at the SAME rate as the medication bolus, according to guidelines found in the PDTM or per IV bolus medication policy. (See Rationale for Flushing with NS after Administering an IV Medication.)
|
Always check hospital policy on the amount of flush and type of solution when using a saline lock for an IV bolus medication.
Flushing the IV line at the same rate as medication delivery ensures that any medication remaining within the IV line is delivered at the correct rate, and avoids giving the patient an accidental bolus of the medication.  Flushing the saline lock clears the medication from the device. Establish positive pressure as per manufacturer’s directions.  If a patient has a central venous catheter, access and flush as per agency policy. |
||
| 12. Dispose of all syringes/filter needles into appropriate puncture-proof containers. | This prevents accidental needle-stick injuries. | ||
| 13. Remove gloves and perform hand hygiene. | This reduces transmission of microorganisms.
 |
||
| 14. Document as per agency protocol. | Document the time, reason, drug, dose, effect, and any adverse reactions. | ||
| 15. Observe for expected therapeutic effect and for adverse effects. | The patient needs to be evaluated and monitored, especially for high-alert medications. IV medications act rapidly. | ||
| Data source: Canadian Institute for Health Information, 2009; Clayton et al., 2010; Perry et al., 2014 | |||
Special Considerations:
- Top contributing factors to medication errors include calculation errors, drug preparation errors, human error, and transcription inaccuracy.
- The elderly and the young may be more sensitive to adverse effects.
- With certain medications, creatinine clearance must be assessed prior to administering. Patients with cirrhosis may require a reduction in dosages.
- When a medication dose is given a range (e.g., morphine 2 mg IV q 2-4 hours p.r.n., or as needed), always start with the lowest dose and titrate up. Always assess when the last dose was given and its effectiveness.
Rationale for Flushing with NS after Administering an IV Medication
Flushing a Saline Lock after Administering an IV Medication
Flushing after IV medication administration with compatible IV solution is recommended as per the guidelines in Checklist 60, Checklist 61, and Checklist 62 to ensure that medication left in the extension tubing is administered at the appropriate rate. IV medication must be cleared by flushing at the same rate of administration to avoid the risks related to IV push medications. Because 1 ml of medication is left in the extension tubing, due care in flushing is required for the first ml that clears the extension tubing. The remaining saline flush serves to maintain patency of the line.
Here are some examples of clearing IV medication from extension tubing.
- If morphine (1 mg) is diluted in 1 ml NS and administered over one minute, the subsequent saline flush will be given in this manner: the first 1 ml of a 5 ml saline flush syringe will be delivered over one minute, and the remaining 4 ml will be given slowly at the level of patient comfort.
- If Lasix (40 mg) is given in a 4 ml volume and administered over two minutes, the subsequent saline flush will be given in this manner: the first 1 ml of a 5 ml saline flush syringe will be delivered over 30 seconds, and the remaining 4 ml will be given slowly at the level of patient comfort.
Flushing the Primary IV Line after Administering an IV Medication through an IV Port
When flushing an IV line after administering an IV medication, the following applies:
- The volume in the IV tubing from the Max Plus saline lock to the first port is also 1 ml. Take this additional volume into account when flushing after a medication is given via this port.
- It is NOT recommended to speed up the IV solution, because medication in the line would be administered too rapidly and is contrary to the manufacturer’s safety recommendation and the PDTM.
- Sudden boluses of some medications may cause mild to severe adverse effects, such as hypotension and toxicity (Clayton et al., 2010).
Checklist 61 lists the steps to administering an IV medication through an existing IV line with compatible IV solution. Review the preparation questions for intravenous medication in Table 7.9 prior to the medication administration.
Checklist 61: Administering an IV medication (with Compatible IV Solution)Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety Considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Prepare one medication for one patient at the correct time as per agency policy. Review the physician’s order, PDTM, and MAR for the correct order and guidelines. Math calculations may be required to determine the correct dose to prepare the medication. | Always apply the SEVEN rights x 3 of medication administration.
Review the agency policy if a medication is a stat, first-time, loading dose, or a one-time dose. Some agencies require that high-alert medications be double-checked by a second health care provider. Always follow agency policies. After preparing the medication, always label the medication syringe with the patient name, date, time, medication and dose concentration (e.g. morphine 2 mg/ml), dose, and your initials. Never leave the syringe unattended. |
||
| 2. Create privacy if possible. | This provides comfort to patient. | ||
| 3. Confirm patient ID using two patient identifiers (e.g., name and date of birth) AND compare the MAR printout with the patient’s wristband to confirm patient ID. | This ensures you have the correct patient and complies with agency standard for patient identification.
 |
||
| 4. Check allergy band for any allergies, and ask patient about type and severity of reaction. | This ensures allergy status is correct on the MAR and on patient allergy band. | ||
| 5. Discuss purpose, action, and possible side effects of the medication. Provide patient an opportunity to ask questions. Encourage patient to report discomfort at the IV site (pain, swelling, or burning). | Keeping patient informed of what is being administered helps decrease anxiety. | ||
| 6. Perform hand hygiene and apply non-sterile gloves. | Hand hygiene prevents the transmission of microorganisms.
 |
||
| 7. Select IV access port closest to the patient. |
 |
||
| 8. Clean port in a circular motion with an alcohol swab for 15 seconds. Allow to dry. | This prevents introduction of microorganisms by the syringe.
 |
||
| 9. Attach syringe (without needle) to IV line using needleless system.
If running primary IV solution is medication (e.g., heparin, morphine, pantaloc, insulin, or blood or blood products), do not flush. Start another saline lock on the opposite arm. |
Using a needleless system prevents needle-stick injuries.
 Never administer a medication using a filter needle. |
||
| 10. If IV solution is on an IV pump, pause the device. Pinch IV tubing above the lowest access port or use blue slider clamp. | This prevents the IV medication from travelling up the IV line.
  |
||
| 11. Inject medication at the recommended rate according to agency policy. Use a timer to monitor time. Use a push-pause method to inject the medication. | This ensures safe medication administration at the correct rate. Rapid injection of IV medications can be fatal.
 |
||
| 12. Remove used medication syringe. Remove air from prefilled NS syringe and attach to the same IV port.
Flush (3 to 5 ml) at the SAME rate as the medication bolus, according to guidelines found in the PDTM or per IV bolus medication policy. (See Rationale for Flushing with NS after Administering an IV Medication.)
|
No needle should be present with a needleless system.
   |
||
| 13. Unpinch/unclamp the IV tubing and ensure the IV is infusing at the correct rate. Restart IV infusion device as required. |
 |
||
| 14. Dispose of all syringes/filter needles into appropriate puncture-proof containers if required. | This prevents accidental needle-stick injuries. | ||
| 15. Remove gloves and perform hand hygiene. | This reduces transmission of microorganisms.
 |
||
| 16. Document as per agency protocol. | Document time, reason, drug, dose, therapeutic effect, and any adverse reactions. | ||
| 17. Evaluate the patient for therapeutic effect and adverse reactions according to appropriate time frame (onset and peak of medication). | Observations provide additional safety measures, especially for high-alert medications. IV medications act rapidly. | ||
| Data source: Berman & Snyder, 2016; Canadian Institute for Health Information, 2009; Clayton et al., 2010; Perry et al., 2014; Workers Compensation Act, 2015 | |||
Special Considerations:
- Top contributing factors to medication errors include calculation errors, drug preparation errors, human error, and transcription inaccuracy. Be diligent in preparing intravenous medications.
- The elderly and the young may be more sensitive to adverse effects of certain intravenous medications.
- With certain medications, creatinine clearance must be assessed prior to administering. Patients with cirrhosis may require a reduction in dosage.
- When a medication dose is given a range (e.g., morphine 2 mg IV q 2 -4 hours p.r.n.), always start with the lowest dose and titrate up. Always assess when the last medication dose was given.
Checklist 62 reviews the steps to administer an IV medication through an existing IV line with incompatible IV solution. Review the preparation questions for intravenous medication in Table 7.9 prior to the medication administration.
Checklist 62: Administering an IV Medication (with Incompatible IV Solution)Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety Considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Prepare one medication for one patient at the correct time as per agency policy. Review the physician orders, PDTM, and MAR for the correct order and guidelines. Math calculations may be required to determine the correct dose to prepare the medication. | Always apply the SEVEN rights x 3 of medication administration.
Review the agency policy if a medication is a stat, first-time, loading dose, or a one-time dose. Some agencies require that high-alert medications be double-checked by a second health care provider. Always follow agency policies. After preparing the medication, always label the medication syringe with the patient name, date, time, medication and dose concentration (e.g. morphine 2 mg/ml), dose, and your initials. Never leave the syringe unattended. |
||
| 2. Create privacy if possible. | This provides comfort to patient. | ||
| 3. Confirm patient ID using two patient identifiers (e.g., name and date of birth) AND compare the MAR printout with the patient’s wristband to confirm patient ID. | This ensures you have the correct patient and complies with agency standard for patient identification.
 |
||
| 4. Check allergy band for any allergies, and ask patient about type and severity of reaction. | This ensures allergy status is correct on the MAR and on patient allergy band. | ||
| 5. Discuss purpose, action, and possible side effects of the medication. Provide patient an opportunity to ask questions. Encourage patient to report discomfort at the IV site (pain, swelling, or burning). | Keeping patient informed of what is being administered helps decrease anxiety. | ||
| 6. Perform hand hygiene and apply non-sterile gloves. | Hand hygiene prevents the transmission of microorganisms.
 |
||
| 7. Clamp or pinch the IV line, and pause the infusion pump if required. | Always ensure the needle insertion site is patent, free from redness and swelling.
Always check agency policy to ensure an IV solution or medication can be stopped temporarily.   Some IV solutions may not be stopped. If unable to temporarily stop an IV solution or IV medication, start a new IV site. |
||
| 8. Clean the lowest port on the IV tubing with an alcohol swab in a circular motion for 15 seconds. Allow to dry. Clamp IV tubing above the lowest port on the IV tubing. | This prevents the transmission of microorganisms.
 |
||
| 9. Flush the IV line with 10 ml of normal saline or as per agency policy. | This step clears the IV line to prevent any mixing of incompatible medications.
 If running primary IV solution is medication (e.g., heparin, morphine, pantaloc, or insulin) or blood or blood products, do not flush. Start another saline lock on the opposite arm. |
||
| 10. Inject medication at the recommended rate according to agency policy. Use timer with second hand to time injection. Use a push-pause method to inject the medication. | Medications can be given safely when guidelines are followed. This ensures the medication is delivered at proper intervals according to agency policy.
 |
||
| 11. Remove used medication syringe. Remove air from prefilled NS syringe and attach to the same IV port.
Flush (3 to 5 ml) at the SAME rate as the medication bolus, according to guidelines found in the PDTM or per IV bolus medication policy. (See Rationale for Flushing with NS after Administering an IV Medication.) |
Flushing at the same rate prevents patient from accidentally receiving a bolus of the medication. Flushing also ensures the line is patent and clears the IV line of all incompatible medications.
 |
||
| 12. Unclamp/unpinch IV line and restart IV infusion device as required. Recheck infusion rate if IV solution is running by gravity. | Rechecking infusion rate prevents accidental fluid overload and keeps patient safe.
 |
||
| 13. Dispose of all syringes/filter needles into appropriate puncture-proof containers. | This prevents accidental needle-stick injuries. | ||
| 14. Remove gloves and perform hand hygiene. | This reduces the transmission of microorganisms.
 |
||
| 15. Document as per agency protocol. | Document time, reason, drug, dose, effect, and any adverse reactions. | ||
| 16. Evaluate the patient’s response to the medication in the appropriate time frame. | Observe patient for expected therapeutic effects and adverse reactions. | ||
| Data source: Berman & Snyder, 2016; Canadian Institute for Health Information, 2009; Clayton et al., 2010; Perry et al., 2014 | |||
Special considerations:
- Top contributing factors to medication errors include calculation errors, drug preparation errors, human error, and transcription inaccuracy.
- The elderly and the young may be more sensitive to adverse effects.
- With certain medications, creatinine clearance must be assessed prior to administering. Patients with cirrhosis may require a reduction in dosages.
- When a medication dose is given a range (e.g., morphine 2 mg IV q 2 -4 hours p.r.n.), always start with the lowest dose and titrate up. Always assess when the last dose was given.
Critical Thinking Exercises
- What resource could you consult to determine the onset, peak, and duration of morphine IV?
- What information should be on the label of an IV medication syringe?

