Sterile procedures are required before and during specific patient care activities to maintain an area free from microorganisms and to prevent infection. Performing a surgical hand scrub, applying sterile gloves, and preparing a sterile field are ways to prevent and minimize infection during surgeries or invasive procedures.
Surgical Hand Scrub
Skin is a major source of microorganisms and a major source of contamination in the OR setting (CDC, 2010). Since skin cannot be sterilized, members of the surgical team must wear sterile gloves. The purpose of the surgical hand scrub is to significantly reduce the number of skin bacteria found on the hands and arms of the OR staff (Kennedy, 2013). A surgical hand scrub is an antiseptic surgical scrub or antiseptic hand rub that is performed prior to donning surgical attire (Perry et al., 2014) and lasts two to five minutes, depending on the product used and hospital policy. Studies have shown that skin bacteria rapidly multiply under surgical gloves if hands are not washed with an antimicrobial soap, whereas a surgical hand scrub will inhibit growth of bacteria under gloved hands (Kennedy, 2013).
Types of surgical hand scrubs
Surgical hand scrub techniques and supplies to clean hands will vary among health care agencies. Most protocols will require a microbial soap-and-water, three- to five-minute hand scrub procedure. Some agencies may use an approved waterless hand scrub product. See Checklist 11 for the steps to follow when scrubbing with medicated soap.
Applying Sterile Gloves
Sterile gloves are gloves that are free from all microorganisms. They are required for any invasive procedure and when contact with any sterile site, tissue, or body cavity is expected (PIDAC, 2012). Sterile gloves help prevent surgical site infections and reduce the risk of exposure to blood and body fluid pathogens for the health care worker. Studies have shown that 18% to 35% of all sterile gloves have tiny holes after surgery, and up to 80% of the tiny puncture sites go unnoticed by the surgeon (Kennedy, 2013). Double gloving is known to reduce the risk of exposure and has become common practice, but does not reduce the risk of cross-contamination after surgery (Kennedy, 2013).
To apply sterile gloves, follow the steps in Checklist 12.
Checklist 12: Donning Sterile GlovesDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Remove all jewellery. | Jewellery harbours more microorganisms than do hands.
 |
||
| 2. No artificial nails, extenders, or chipped nail polish should be worn. | Artificial nails, extenders, and chipped nail polish can harbour additional microorganisms. | ||
| 3. Inspect hands for sores and abrasions. Cover or report to supervisor as required. | Open sores can harbour microorganisms. | ||
| 4. Ensure sleeves are at least two to three inches above the elbows. | This step prevents sleeves from becoming moist, and prevents the transfer of microorganisms from the sleeves. | ||
| 5. Clean hands with ABHR or soap and water. | This step decreases the bacterial count on hands and prevents contamination of sterile equipment.
 |
||
| 6. Clean surface to open sterile field and raise its height to waist level. | All sterile items must be kept above waist level. | ||
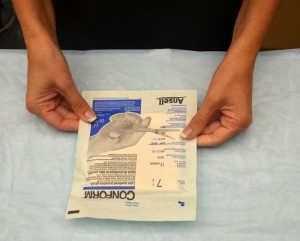
| 7. Inspect packaging for sterility. | All sterile items must be checked for sterility prior to use. Always examine sterile glove packaging for expiry date, intactness, and tears. The package should be dry. Sterile gloves have outer packaging that must be removed prior to starting the procedure of applying sterile gloves.
 |
||
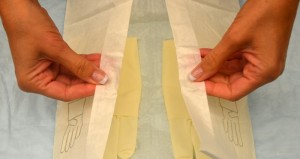
| 8. Open sterile packaging by peeling open the top seam and pulling down. | Open sterile packaging without contaminating inner package.
 |
||
| 9. Place inner package on working surface and open up to see right and left gloves. Start with dominant hand first. Open packaging. | This step prepares sterile surface to perform sterile application of gloves.
   |
||
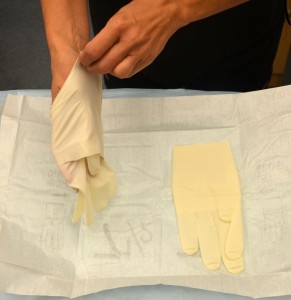
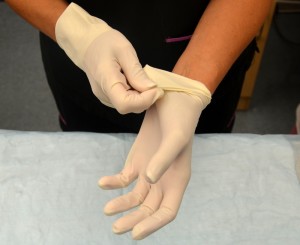
| 10. Pick up glove for dominant hand by touching the inside cuff of the glove. Do not touch the outside of the glove. Pull glove completely over dominant hand. | This step allows ease of application.
   |
||
| 11. Insert gloved hand into the cuff of the remaining glove. Pull remaining glove on non-dominant hand and insert fingers. Adjust gloves if necessary. | This ensures proper fit of gloves.
   |
||
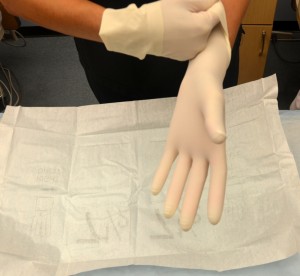
| 12. Once gloves are on, interlock gloved hands and keep at least six inches away from clothing, keeping hands above waist level and below the shoulders. | This step prevents the accidental touching of non-sterile objects or the front of the gown.
 |
||
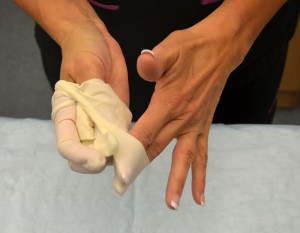
| 13. To remove gloves, grasp the outside of the cuff or palm of glove and gently pull the glove off, turning it inside out and placing it into gloved hand. | Doing this, prevents the contamination of the hand when removing glove.
   |
||
| 14. Take ungloved hand, place fingers inside the other glove, and pull glove off inside out. | This step prevents the contamination of gloved hand touching ungloved hand.
  |
||
| 15. Perform hand hygiene. | This removes powder from the gloves, which can irritate the skin; it also prevents contamination from potential pinholes in the gloves.
 |
||
| Data source: ATI, 2015b; Berman & Snyder, 2016; Kennedy, 2013; Perry et al., 2014; Rothrock, 2014 | |||
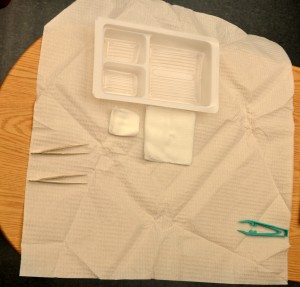
Setting up a Sterile Field
Aseptic procedures require a sterile area in which to work with sterile objects. A sterile field is a sterile surface on which to place sterile equipment that is considered free from microorganisms (Perry et al., 2014). A sterile field is required for all invasive procedures to prevent the transfer of microorganisms and reduce the potential for surgical site infections. Sterile fields can be created in the OR using drapes, or at the bedside using a prepackaged set of supplies for a sterile procedure or wound care. Many sterile kits contain a waterproof inner drape that can be set up as part of the sterile field. Sterile items can be linen wrapped or paper wrapped, depending on whether they are single- or multi-use. Always check hospital policy and doctor orders if a sterile field is required for a procedure. See Checklist 13 for the steps for preparing a sterile field.
Checklist 13: Preparing a Sterile FieldDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Perform hand hygiene, gather supplies, check equipment for sterility, and gather additional supplies (gauze, sterile cleaning solution, sterile gloves, etc.). | Gathering additional supplies at the same time will help avoid leaving the sterile field unattended. Prepackaged sterile kits may not have all the supplies required for each procedure.
 |
||
| 2. Place package on clean, dry, waist-level table. | A clean, dry surface is required to set up a sterile field.
Items below waist level are considered contaminated. Prepare sterile field as close to the time of procedure as possible.  |
||
| 3. Remove the outside sterile packaging and discard. | This allows more space to set up a sterile field. | ||
| 4. Grab the outer surface’s outermost tip (corner of folded drape) and open the flap away from you. | The one-inch border on the sterile field is considered non-sterile. Make sure your arm is not over the sterile field.
The inside of the sterile packaging is your sterile drape. Stand away from your sterile field when opening sterile packaging. 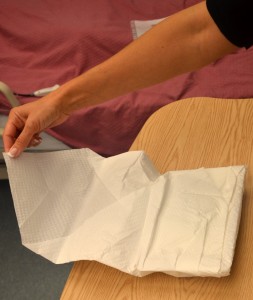 |
||
| 5. Grab the side flaps and open outwards, and let it lie flat on the table. | Touch only the one-inch border on the sterile field. Do not reach over the sterile field.
  |
||
| 6. Grasping the outermost corner, pull the last flap toward you, and lay it flat on the table. | This step creates an open sterile field.
  |
||
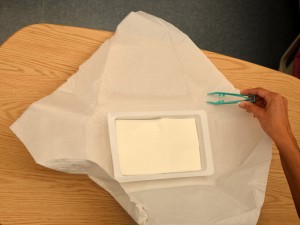
| 7. Using sterile forceps, rearrange sterile equipment on the sterile field in order of usage. | This step saves time for completing sterile procedure; it also limits the amount of time the sterile field is exposed to air.
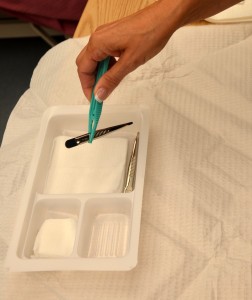  |
||
| Adding Sterile Items to a Sterile Field | |||
| 8. Supplies can be opened (following packaging directions), then gently dropped onto the sterile field.
|
Gently drop items onto the sterile field or use sterile forceps to place sterile items onto the field.
If using equipment wrapped in linen, ensure sterility by checking the tape for date and to view chemical indicator (stripes on the tape ensure sterility has been achieved). When using paper-wrapped items, they should be dry and free from tears. Confirm expiry date. Do not flip or toss objects onto the sterile field.  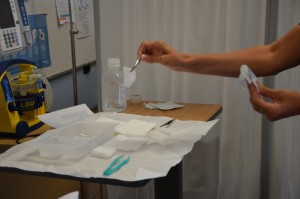 |
||
9. Add solution to the sterile tray by pouring the solution carefully into the receptacle:
|
Do not touch the edge of the solution receptacle. Place the receptacle near the edge of the sterile field.
  This ensures the sterility of the solution and the use of the correct solution. It also ensures the bottle of solution does not come in contact with the sterile field. Lastly, it verifies the type of solution required for the procedure. Be careful not to drip solution onto the sterile field, causing contamination. (When liquid permeates a sterile field it is called strike through.) |
||
| Data source: ATI, 2015c; Berman & Snyder, 2016; Kennedy, 2013; Perry et al., 2014; Rothrock, 2014 | |||
Sterile Attire in the OR
Wearing sterile surgical attire (sterile gowns, closed gloving, and masks) and PPE is essential to keep the restricted and semi-restricted areas clean and to minimize sources of microbial transmission and contamination. It is important to minimize the patient’s exposure to the surgical team’s skin, mucous membranes, and hair by the proper application of surgical attire. An extensive list of recommendations for surgical attire can be located on the Association of periOperative Registered Nurses (AORN) website at Recommendations for surgical attire (Braswell & Spruce, 2012).
Critical Thinking Exercises
- Name four differences between a medical hand wash with soap and water and a surgical hand scrub.
- When preparing a sterile field, is the first flap open toward the health care provider or away from the health care provider?
- Name two reasons for performing hand hygiene before and after applying sterile gloves.


