3.6 Navigating Mood Disorders
Module Overview

We will discuss matters related to mood disorders including their clinical presentation, epidemiology, comorbidity, etiology, and treatment options. Our discussion will introduce Major Depressive Disorder, Persistent Depressive Disorder (formerly Dysthymia), Bipolar I disorder, Bipolar II disorder, and Cyclothymic disorder. We will also cover major depressive, manic, and hypomanic episodes. We will cover Bipolar and REeated Disorders and Depressive Disorders from the DSM 5-TR.
Learning Objectives
- Describe how depressive disorders present.
- Describe how bipolar disorders present.
- Describe the epidemiology of mood disorders.
- Describe comorbidity in relation to mood disorders.
- Describe the etiology of mood disorders.
- Describe treatment options for mood disorders.
CLINICAL PRESENTATION – DEPRESSIVE DISORDERS
Depressive Disorders Learning Objectives
- Distinguish the two distinct groups of mood disorders.
- Identify and describe the two types of depressive disorders.
- Classify symptoms of depression.
- Describe premenstrual dysphoric disorder
Within mood disorders are two distinct groups—individuals with depressive disorders and individuals with bipolar disorders. The key difference between the two mood disorder groups is episodes of mania/hypomania. More specifically, in bipolar I disorder, the individual experiences a manic episode that “may have been preceded by and may be followed by hypomanic or major depressive episodes” (1) whereas for bipolar II disorder, the individual has experienced in the past or is currently experiencing a hypomanic episode and has experienced in the past or is currently experiencing a major depressive episode. In contrast, individuals presenting with a depressive disorder have never experienced a manic or hypomanic episode.
Types of Depressive Disorders
The two most common types of depressive disorders are major depressive disorder (MDD) and persistent depressive disorder (PDD). Persistent depressive disorder, which in the DSM-5 now includes the diagnostic categories of dysthymia and chronic major depression, is a continuous and chronic form of depression. While the symptoms of PDD are very similar to MDD, they are usually less acute, as symptoms tend to ebb and flow over a long period (i.e., more than two years). Major depressive disorder, on the other hand, has discrete episodes lasting at least two weeks in which there are substantial changes in affect, cognition, and neurovegetative functions (2).
It should be noted that after a careful review of the literature, premenstrual dysphoric disorder, was moved from “Criteria Sets and Axes Provided for Future Study” in the DSM-IV to Section II of DSM-5 as the disorder was confirmed as a “specific and treatment-responsive form of depressive disorder that begins sometime following ovulation and remits within a few days of menses and has a marked impact on functioning” (2).
The DSM-5 also added a new diagnosis, disruptive mood dysregulation disorder (DMDD), for children up to 12 years of age, to deal with the potential for overdiagnosis and treatment of bipolar disorder in children, both in the United States and internationally. Children with DMDD present with persistent irritability and frequent episodes of extreme behavioral dyscontrol and so develop unipolar, not bipolar, depressive disorders or anxiety disorders as they move into adolescence and adulthood.
For a discussion of DMDD, please visit our sister book, Behavioral Disorders of Childhood:
https://opentext.wsu.edu/behavioral-disorders-childhood/ (3)
Symptoms Associated with Depressive Disorders
When making a diagnosis of depression, there are a wide range of symptoms that may be present. These symptoms can generally be grouped into four categories: mood, behavioural, cognitive, and physical symptoms.
Mood
While clinical depression can vary in its presentation among individuals, most, if not all individuals with depression will report significant mood disturbances such as a depressed mood for most of the day and/or feelings of anhedonia, which is the loss of interest in previously interesting activities.
Behavioural
Behavioural issues such as decreased physical activity and reduced productivity—both at home and work—are often observed in individuals with depression. This is typically where a disruption in daily functioning occurs as individuals with depressive disorders are unable to maintain their social interactions and employment responsibilities.
Cognitive
It should not come as a surprise that there is a serious disruption in cognitions as individuals with depressive disorders typically hold a negative view of themselves and the world around them. They are quick to blame themselves when things go wrong, and rarely take credit when they experience positive achievements. Individuals with depressive disorders often feel worthless, which creates a negative feedback loop by reinforcing their overall depressed mood. They also report difficulty concentrating on tasks, as they are easily distracted from outside stimuli. This assertion is supported by research that has found individuals with depression perform worse than those without depression on tasks of memory, attention, and reasoning (4). Finally, thoughts of suicide and self-harm do occasionally occur in those with depressive disorders; this will be discussed in the epidemiology section in more detail.
Physical
Changes in sleep patterns are common in those experiencing depression with reports of both hypersomnia and insomnia. Hypersomnia, or excessive sleeping, often impacts an individual’s daily functioning as they spend the majority of their time sleeping as opposed to participating in daily activities (i.e., meeting up with friends, getting to work on time). Reports of insomnia are also frequent and can occur at various points throughout the night including difficulty falling asleep, staying asleep, or waking too early with the inability to fall back asleep before having to wake for the day. Although it is unclear whether symptoms of fatigue or loss of energy are related to insomnia issues, the fact that those experiencing hypersomnia also report symptoms of fatigue suggests that these symptoms are a component of the disorder rather than a secondary symptom of sleep disturbance.
Additional physical symptoms, such as a change in weight or eating behaviours, are also observed. Some individuals who are experiencing depression report a lack of appetite, often forcing themselves to eat something during the day. On the contrary, others overeat, often seeking “comfort foods,” such as those high in carbohydrates. Due to these changes in eating behaviours, there may be associated changes in weight.
Finally, psychomotor agitation or retardation, which is the purposeless or slowed physical movement of the body (i.e., pacing around a room, tapping toes, restlessness, etc.) is also reported in individuals with depressive disorders.
Diagnostic Criteria and Features for Depressive Disorder
Major depressive disorder (MDD). According to the DSM-5-TR (APA, 2022), to meet the criteria for a diagnosis of major depressive disorder, an individual must experience at least five symptoms across the four categories discussed above, and at least one of the symptoms is either 1) a depressed mood most of the day, almost every day, or 2) loss of interest or pleasure in all, or most, activities, most of the day, almost every day. These symptoms must be present for at least two weeks and cause clinically significant distress or impairment in important areas of functioning such as social and occupational. The DSM-5 cautions that responses to a significant loss (such as the death of a loved one, financial ruin, and discovery of a serious medical illness or disability), can lead to many of the symptoms described above (i.e., intense sadness, rumination about the loss, insomnia, etc.) but this may be the normal response to such a loss. Though the individual’s response resembles a major depressive episode, clinical judgment should be utilized in making any diagnosis and be based on the clinician’s understanding of the individual’s personal history and cultural norms related to how members should express distress in the context of loss.
Persistent depressive disorder (PDD). For a diagnosis of persistent depressive disorder, an individual must experience a depressed mood for most of the day, for more days than not, for at least two years (APA, 2022). This feeling of a depressed mood is also accompanied by two or more additional symptoms, to include changes in appetite, insomnia or hypersomnia, low energy or fatigue, low self-esteem, feelings of hopelessness, and poor concentration or difficulty with decision making. The symptoms taken together cause clinically significant distress or impairment in important areas of functioning such as social and occupational and these impacts can be as great as or greater than MDD. The individual may experience a temporary relief of symptoms; however, the individual will not be without symptoms for more than two months during this two-year period.
Making Sense of the Disorders
In relation to depressive disorders, note the following:
- Diagnosis MDD …… if symptoms have been experienced for at least two weeks and can be regarded as severe
- Diagnosis PDD … if the symptoms have been experienced for at least two years and are not severe
Premenstrual dysphoric disorder. In terms of premenstrual dysphoric disorder, the DSM-5-TR states in the majority of menstrual cycles, at least five symptoms must be present in the final week before the onset of menses, being improving with a few days after menses begins, and disappear or become negligible in the week postmenses. Individuals diagnosed with premenstrual dysphoric disorder must have one or more of the following: increased mood swings, irritability or anger, depressed mood, or anxiety/tension. Additionally, they must have one or more of the following to reach a total of five symptoms: anhedonia, difficulty concentrating, lethargy, changes in appetite, hypersomnia or insomnia, feelings of being overwhelmed or out of control, and/or experience breast tenderness or swelling. The symptoms lead to issues at work or school (i.e., decreased productivity and efficiency), within relationships (i.e., discord in the intimate partner relationship or with children, friends, or other family members), and with usual social activities (i.e., avoidance of the activities).
Key Takeaways
You should have learned the following in this section:
- Mood disorder fall into one of two groups – depressive or bipolar disorders – with the key distinction between the two being episodes of mania/hypomania.
- Symptoms of depression fall into one of four categories – mood, behavioural, cognitive, and physical.
- Persistent Depressive Disorder shares symptoms with Major Depressive Disorder though they are usually not as severe and ebb and flow over a period of at least two years.
- Premenstrual dysphoric disorder presents as mood lability, irritability, dysphoria, and anxiety symptoms occurring often during the premenstrual phase of the cycle and remit around the beginning of menses or shortly thereafter.
Review Questions
-
- What are the different categories of mood disorder symptoms? Identify the symptoms within each category.
- What are the key differences in a major depression and a persistent depressive disorder diagnosis?
- What is premenstrual dysphoric disorder?
CLINICAL PRESENTATION – BIPOLAR AND RELATED DISORDERS
Bipolar Disorders Learning Objectives
- Distinguish the forms bipolar disorder takes.
- Contrast a manic episode with a hypomanic episode
- Define cyclothymic disorder.
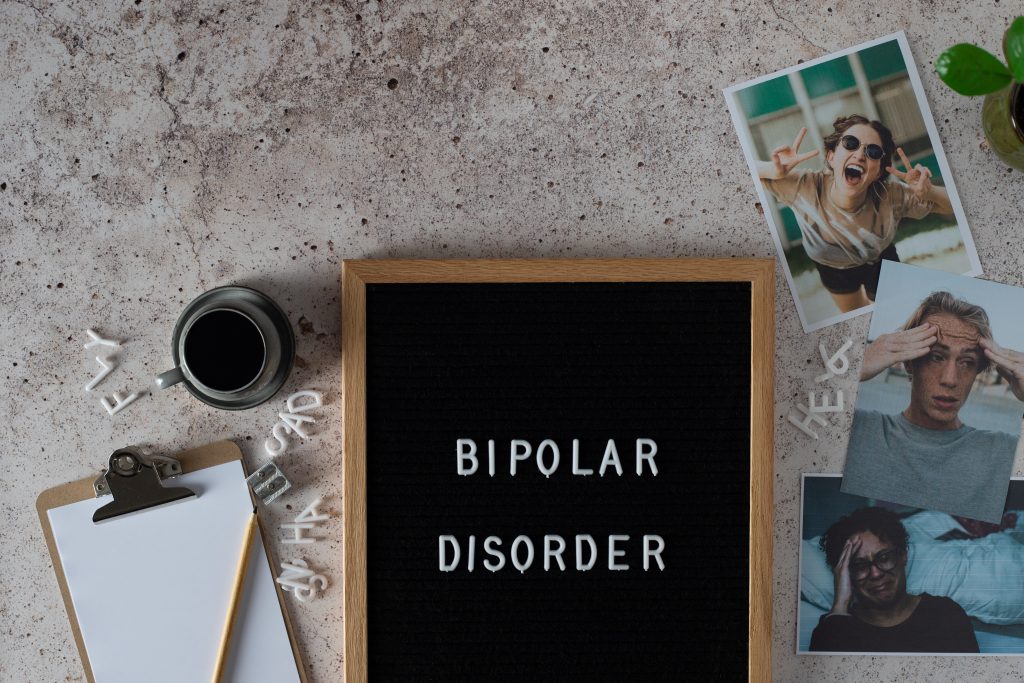
Distinguishing Bipolar I and II Disorders
According to the DSM-5 (APA, 2022), there are two types of Bipolar Disorder- Bipolar I and Bipolar II. A diagnosis of Bipolar I Disorder is made when there is at least one manic episode. This manic episode can be preceded by or followed by a hypomanic or major depressive episode, however, diagnostic criteria for a manic episode are the only criteria that need to be met for a Bipolar I diagnosis. A diagnosis of Bipolar II Disorder is made when there is a current or history of a hypomanic episode and a current or past major depressive episode. In simpler words, if an individual has ever experienced a manic episode, they qualify for a Bipolar I diagnosis; however, if the criteria have only been met for a hypomanic episode, the individual qualifies for a Bipolar II diagnosis.
Making Sense of the Disorders
In relation to bipoloar I and II disorders, note the following:
- Diagnosis bipolar I disorder …. if an individual has ever experienced a manic episode
- Diagnosis bipolar II disorder … if the criteria has only been met for a hypomanic episode
Manic Episode
Manic episode. The key feature of a manic episode is a specific period in which an individual reports abnormal, persistent, or expansive irritable mood for nearly all day, every day, for at least one week (APA, 2022). Additionally, the individual will display increased activity or energy during this same time. With regards to mood, an individual in a manic episode will appear excessively happy, often engaging haphazardly in sexual or interpersonal interactions. They also display rapid shifts in mood, also known as mood lability, ranging from happy, neutral, to irritable. At least three of the symptoms described below (four if the mood is only irritable) must be present and represent a noticeable change in the individual’s typical behaviour.
Inflated self-esteem or grandiosity (Criterion B1) is present during a manic episode. Occasionally these inflated self-esteem levels can appear delusional. For example, individuals may believe they are friends with a celebrity, do not need to abide by laws, or even perceive themselves as God. They also engage in multiple overlapping new projects (Criteria B6 and 7), often initiated with no prior knowledge about the topic, and engaged in at unusual hours of the day.
Despite the increased activity level, individuals experiencing a manic episode also require a decreased need for sleep (Criterion B2), sleeping as little as a few hours a night yet still feeling rested. Reduced need for sleep may also be a precursor to a manic episode, suggesting that a manic episode is to begin imminently. It is not uncommon for those experiencing a manic episode to be more talkative than usual. It can be difficult to follow their conversation due to the quick pace of their talking, as well as tangential storytelling. Additionally, they can be difficult to interrupt in conversation, often disregarding the reciprocal nature of communication (Criterion B3). If the individual is more irritable than expansive, speech can become hostile and they engage in tirades, particularly if they are interrupted or not allowed to engage in an activity they are seeking out (APA, 2022).
Based on their speech pattern, it should not be a surprise that racing thoughts and flights of ideas (Criterion B4) also present during manic episodes. Because of these rapid thoughts, speech may become disorganized or incoherent. Finally, individuals experiencing a manic episode are distractable (Criterion B5).
Hypomanic Episode
Hypomanic episode. As mentioned above, for a bipolar II diagnosis, an individual must report symptoms consistent with a major depressive episode and at least one hypomanic episode. An individual with bipolar II disorder must not have a history of a manic episode—if there is a history of mania, the diagnosis will be diagnosed with bipolar I. A hypomanic episode is like a manic episode in that the individual will experience abnormally and persistently elevated, expansive, or irritable mood and energy levels, however, the behaviours are not as extreme as in mania. Additionally, behaviours consistent with a hypomanic episode must be present for at least four days, compared to the one week in a manic episode.
Making Sense of the Disorders
Take note of the following in relation to manic and hypomanic episodes:
- A manic episode is severe enough to cause impairments in social or occupational functioning and can lead to hospitalization to prevent harm to self or others.
- A hypomanic episode is NOT severe enough to cause such impairments or hospitalization.
Cyclothymic Disorder
Notably, there is a subclass of individuals who experience numerous periods with hypomanic symptoms that do not meet the criteria for a hypomanic episode and mild depressive symptoms (i.e., do not fully meet criteria for a major depressive episode). These individuals are diagnosed with cyclothymic disorder (APA, 2022). Presentation of these symptoms occur for two or more years and are typically interrupted by periods of normal mood not lasting more than two months at a time. The symptoms cause clinically significant distress or impairment in important areas of functioning, such as social and occupational. While only a small percentage of the population develops cyclothymic disorder, it can eventually progress into bipolar I or bipolar II disorder.
Key Takeaways
You should have learned the following in this section:
- An individual is diagnosed with bipolar I disorder if they have ever experienced a manic episode and are diagnosed with bipolar II disorder if the criteria has only been met for a hypomanic episode.
- A manic episode is characterized by a specific period in which an individual reports abnormal, persistent, or expansive irritable mood for nearly all day, every day, for at least one week.
- A hypomanic episode is characterized by abnormally and persistently elevated, expansive, or irritable mood and energy levels, though not as extreme as in mania, and must be present for at least four days. It is also not severe enough to cause impairments or hospitalization.
- Cyclothymic disorder includes periods of hypomanic and mild depressive symptoms without meeting the criteria for a depressive episode which lasts two or more years and is interrupted by periods of normal moods.
Review Questions
- What is the difference between bipolar I and II disorder?
- What are the key diagnostic differences between a hypomanic and manic episode?
- What is cyclothymic disorder?
EPIDEMIOLOGY
Epidemiology Learning Objectives
- Describe the epidemiology of depressive disorders.
- Describe the epidemiology of bipolar disorders.
- Describe the epidemiology of suicidality.
Depressive Disorders

According to the DSM-5-TR (APA, 2022), the 12-month prevalence rate for major depressive disorder is approximately 7% within the United States. Recall that DSM-5 persistent depressive disorder is a blend of DSM-IV dysthymic disorder and chronic major depressive disorder. The prevalence rate for DSM-IV dysthymic disorder is much lower than MDD, with a 0.5% rate among adults in the United States, while DSM-IV chronic major depressive disorder is 1.5%.
As well, individuals in the 18- to 29- year-old age bracket report the highest rates of MDD than any other age group. Women experience about twofold higher rates than men of MDD, especially between menarche and menopause (APA, 2022). The estimated lifetime prevalence for major depressive disorder in women is 21.3% compared to 12.7% in men (5). Regrading DSM-IV dysthymic disorder and chronic major depressive disorder, the prevalence among women is 1.5 and 2 times greater than the prevalence for men for each of these diagnoses, respectively (APA, 2022).
Bipolar Disorders
The 12-month prevalence of bipolar I disorder in the United States is 1.5% and did not differ statistically between men and women. In contrast, bipolar II disorder has a prevalence rate of 0.8% in the United States and 0.3% internationally (APA, 2022), and some clinical samples suggest it is more common in women, with approximately 80-90% of individuals with rapid-cycling episodes being women (6). Childbirth may be a specific trigger for a hypomanic episode, occurring in 10-20% of women in nonclinical settings and most often in the early postpartum period.
Suicidality
Individuals with a depressive disorder have a 17-fold increased risk for suicide over the age- and sex-adjusted general population rate. Features associated with an increased risk for death by suicide include anhedonia, living alone, being single, disconnecting socially, having access to a firearm, early life adversity, sleep disturbance, feelings of hopelessness, and problems with decision making. Women attempt suicide at a higher rate though men are more likely to complete suicide. Finally, the premenstrual phase is considered a risk period for suicide by some (APA, 2022).
In terms of bipolar disorders, the lifetime risk of suicide is estimated to be 20- to 30- fold greater than in the general population and 5-6% of individuals with bipolar disorder die by suicide. Like depressive disorders, women attempt suicide at a higher rate though lethal suicide is more common in men with bipolar disorder. About 1/3 of individuals with bipolar II disorder report a lifetime history of suicide attempt, which is similar in bipolar I disorder, though lethality of attempts is higher in individuals with bipolar II (APA, 2022).
Key Takeaways
You should have learned the following in this section:
- Major depressive disorder is experienced by about 7% of the population in the United States, afflicting young adults and women the most.
- Bipolar I disorder afflicts 1.5% and bipolar II disorder afflicts 0.8% of the U.S. population with bipolar II affecting women more than men and no gender difference being apparent for bipolar I.
- Individuals with a depressive disorder have a 17-fold increased risk for suicide while the lifetime risk of suicide for an individual with a bipolar disorder is estimated to be 20- to 30- fold greater than in the general population and 5-6% of individuals with bipolar disorder die by suicide.
Review Questions
- What are the prevalence rates of the mood disorders?
- What gender differences exist in the rate of occurrence of mood disorders?
- How do depressive and bipolar disorders compare in terms of suicidality (attempts and lethality)?
COMORBIDITY
Comorbidity Learning Objectives
- Describe the comorbidity of depressive disorders.
- Describe the comorbidity of bipolar disorders.
Depressive Disorders
Studies exploring depression symptoms among the general population show a substantial pattern of comorbidity between depression and other mental disorders, particularly substance use disorders (7). Nearly three-fourths of participants with lifetime MDD in a large-scale research study also met the criteria for at least one other DSM disorder (7). MDD has been found to co-occur with substance-related disorders, panic disorder, generalized anxiety disorder, PTSD, OCD, anorexia, bulimia, and borderline personality disorder. Gender differences do exist within comorbidities such that women report comorbid anxiety disorders, bulimia, and somatoform disorders while men report comorbid alcohol and substance abuse. In contrast, those with PDD are at higher risk for psychiatric comorbidity in general and for anxiety disorders, substance use disorders, and personality disorders in particular (APA, 2022).
Given the extent of comorbidity among individuals with MDD, researchers have tried to identify which disorder precipitated the other. The majority of studies found that most depression cases occur secondary to another mental health disorder, meaning that the onset of depression is a direct result of the onset of another disorder (8).
Bipolar Disorders
Those with bipolar I disorder typically have a history of three or more mental disorders. The most frequent comorbid disorders include anxiety disorders, alcohol use disorder, other substance use disorder, and ADHD, along with borderline, schizotypal, and antisocial personality disorder.
Bipolar II disorder is more often than not associated with one or more comorbid mental disorders, with anxiety disorders being the most common (38% with social anxiety, 36% with specific phobia, and 30% having generalized anxiety). As with bipolar I, substance use disorders are common with alcohol use (42%) leading the way, followed by cannabis use (20%). Premenstrual syndrome and premenstrual dysphoric disorder are common in women with bipolar II disorder especially (APA, 2022).
Finally, cyclothymic disorder has been found to be comorbid with substance-related disorders and sleep disorders.
Key Takeaways
You should have learned the following in this section:
- Depressive disorders have high comorbidity with substance use disorders, anxiety disorders, ADHD, and substance abuse with these other disorders often causing depression.
- Bipolar disorder has high comorbidity with anxiety disorders, disruptive/impulse-control disorders, and substance abuse disorders.
Review Questions
- What are common comorbidities for the depressive disorder?
- What are common comorbidities for bipolar disorders?
ETIOLOGY
Etiology Learning Objectives
- Describe the biological causes of mood disorders.
- Describe the cognitive causes of mood disorders.
- Describe the behavioural causes of mood disorders.
- Describe the socio-cultural causes of mood disorders.
Biological
Research throughout the years continues to provide evidence that depressive disorders have some biological cause. While it does not explain every depressive case, it is safe to say that some individuals may at least have a predisposition to developing a depressive disorder. Among the biological factors are genetic factors, biochemical factors, and brain structure.
Genetics Like with any disorder, researchers often explore the prevalence rate of depressive disorders among family members to determine if there is some genetic component, whether it be a direct link or a predisposition. If there is a genetic predisposition to developing depressive disorders, one would expect a higher rate of depression within families than that of the general population. Research supports this with regards to depressive disorders as there is nearly a 30% increase in relatives diagnosed with depression compared to 10% of the general population (9). Similarly, there are an elevated prevalence among first-degree relatives for both Bipolar I and Bipolar II disorders as well.
Another way to study the genetic component of a disorder is via twin studies. One would expect identical twins to have a higher rate of the disorder as opposed to fraternal twins, as identical twins share the same genetic make-up, whereas fraternal twins only share roughly 50%, similar to that of siblings. A large-scale study found that if one identical twin was diagnosed with depression, there was a 46% chance their identical twin was diagnosed with depression. In contrast, the rate of depression diagnosis in fraternal twins was only 20%. Despite the fraternal twin rate still being higher than that of a first-degree relative, this study provided enough evidence that there is a strong genetic link in the development of depression (10)
More recently, scientists have been studying depression at a molecular level, exploring possibilities of gene abnormalities as a cause for developing a depressive disorder. While much of the research is speculation due to sampling issues and low power, there is some evidence that depression may be tied to the 5-HTT gene on chromosome 17, as this is responsible for the activity of serotonin (11).
Bipolar disorders share a similar genetic predisposition to that of major depressive disorder. Twin studies within bipolar disorder yielded concordance rates for identical twins at as high as 72%, yet the range for fraternal twins, siblings, and other close relatives ranged from 5-15%. It is important to note that both percentages are significantly higher than that of the general population, suggesting a strong genetic component within bipolar disorder (12). The DSM-5-TR more recently reports heritability estimates around 90% in some twin studies and the risk of bipolar disorder being around 1% in the general population compared to 5-10% in a first-degree relative (APA, 2022).
Biochemical As you will read in the treatment section, there is strong evidence of a biochemical deficit in depression and bipolar disorders. More specifically, low activity levels of norepinephrine and serotonin, have long been documented as contributing factors to developing depressive disorders. This relationship was discovered accidentally in the 1950s when MAOIs were given to tuberculosis patients, and miraculously, their depressive moods were also improved. Soon thereafter, medical providers found that medications used to treat high blood pressure by causing a reduction in norepinephrine also caused depression in their patients (13).
While these initial findings were premature in the identification of how neurotransmitters affected the development of depressive features, they did provide insight as to what neurotransmitters were involved in this system. Researchers are still trying to determine the exact pathways; however, it does appear that both norepinephrine and serotonin are involved in the development of symptoms, whether it be between the interaction between them, or their interaction with other neurotransmitters (14).
Due to the close nature of depression and bipolar disorder, researchers initially believed that both norepinephrine and serotonin were implicated in the development of bipolar disorder; however, the idea was that there was a drastic increase in serotonin during mania episodes. Unfortunately, research supports the opposite. It is believed that low levels of serotonin and high levels of norepinephrine may explain mania episodes (15). Despite these findings, additional research in this area is needed to conclusively determine what is responsible for the manic episodes of bipolar disorder.
Endocrine system. As you may know, the endocrine system is a collection of glands responsible for regulating hormones, metabolism, growth and development, sleep, and mood, among other things. Some research has implicated hormones, particularly cortisol, a hormone released as a stress response, in the development of depression (16). Additionally, melatonin, a hormone released when it is dark outside to assist with the transition to sleep, may also be related to depressive symptoms, particularly during the winter months.
Brain anatomy. Seeing as neurotransmitters have been implicated in the development of depressive disorders, it should not be a surprise that various brain structures have also been identified as contributors to mood disorders. While exact anatomy and pathways are yet to be determined, research studies implicate the prefrontal cortex, the hippocampus, and the amygdala. More specifically, drastic changes in blood flow throughout the prefrontal cortex have been linked with depressive symptoms. Similarly, a smaller hippocampus, and consequently, fewer neurons, has also been linked to depressive symptoms. Finally, heightened activity and blood flow in the amygdala, the brain area responsible for our fight or flight emotions, is also consistently found in individuals with depressive symptoms.
Abnormalities to several brain structures have also been identified in individuals with bipolar disorder; however, what or why these structures are abnormal has yet to be determined. Researchers continue to focus on areas of the basal ganglia and cerebellum, which appear to be much smaller in individuals with bipolar disorder compared to the general public. Additionally, there appears to be a decrease in brain activity in regions associated with regulating emotions, as well as an increase in brain activity among structures related to emotional responsiveness (17). Additional research is still needed to determine precisely how each of these brain structures may be implicated in the development of the bipolar disorder.
Cognitive
The cognitive model, arguably the most conclusive model with regards to depressive disorders, focuses on the negative thoughts and perceptions of an individual. One theory often equated with the cognitive model of depression is learned helplessness. Coined by Martin Seligman (18), learned helplessness was developed based on his laboratory experiment involving dogs. In this study, Seligman restrained dogs in an apparatus and routinely shocked them regardless of their behaviour. The following day, the dogs were placed in a similar apparatus; however, this time they were not restrained and there was a small barrier placed between the “shock” floor and the “safe” floor. What Seligman observed was that despite the opportunity to escape the shock, the dogs flurried for a bit, and then ultimately laid down and whimpered while being shocked.
Based on this study, Seligman concluded that the animals essentially learned that they were unable to avoid the shock the day prior, and therefore, learned that they were helpless in preventing the shocks. When they were placed in a similar environment but had the opportunity to escape the shock, their learned helplessness carried over, and they continued to believe they were unable to escape the shock.
This study has been linked to humans through research on attributional style (19). There are two types of attributional styles—positive and negative. A negative attributional style focuses on the internal, stable, and global influence of daily lives, whereas a positive attributional style focuses on the external, unstable, and specific influence of the environment. Research has found that individuals with a negative attributional style are more likely to experience depression. This is likely due to their negative interpretation of daily events. For example, if something bad were to happen to them, they would conclude that it is their fault (internal), bad things always happen to them (stable), and bad things happen all day to them. Unfortunately, this maladaptive thinking style often takes over an individual’s daily view, thus making them more vulnerable to depression.
In addition to attributional style, Aaron Beck also attributed negative thinking as a precursor to depressive disorders (20, 21, 22). Often viewed as the grandfather of Cognitive-Behavioural Therapy, Beck went on to coin the terms—maladaptive attitudes, cognitive triad, errors in thinking, and automatic thoughts—all of which combine to explain the cognitive model of depressive disorders.
Maladaptive attitudes, or negative attitudes about oneself, others, and the world around them are often present in those with depressive symptoms. These attitudes are inaccurate and often global. For example, “If I fail my exam, the world will know I’m stupid.” Will the entire world really know you failed your exam? Not likely. Because you fail the exam, are you stupid? No. Individuals with depressive symptoms often develop these maladaptive attitudes regarding everything in their life, indirectly isolating themselves from others. The cognitive triad also plays into the maladaptive attitudes in that the individual interprets these negative thoughts about their experiences, themselves, and their futures.
Cognitive distortions, also known as errors in thinking, are a key component in Beck’s cognitive theory. Beck identified 15 errors in thinking that are most common in individuals with depression (see the end of the module). Among the most common are catastrophizing, jumping to conclusions, and overgeneralization. I always like to use my dad (first author’s dad) as an example for overgeneralization. Whenever we go to the grocery store, he always comments about how whatever line he chooses, at every store, it is always the slowest line. Does this happen every time he is at the store? I’m doubtful, but his error in thinking leads to him believing this is true.
Finally, automatic thoughts, or the constant stream of negative thoughts, also lead to symptoms of depression as individuals begin to feel as though they are inadequate or helpless in a given situation. While some cognitions are manipulated and interpreted negatively, Beck stated that there is another set of negative thoughts that occur automatically. Research studies have continually supported Beck’s maladaptive thoughts, attitudes, and errors in thinking as fundamental issues in those with depressive disorders (23)(24). Furthermore, as you will see in the treatment section, cognitive strategies are among the most effective forms of treatment for depressive disorders.
Behavioural
The behavioural model explains depression as a result of a change in the number of rewards and punishments one receives throughout their life. This change can come from work, intimate relationships, family, or even the environment in general. Among the most influential in the field of depression is Peter Lewinsohn. He stated depression occurred in most people due to the reduced positive rewards in their life. Because they were not positively rewarded, their constructive behaviours occurred more infrequently until they stop engaging in the behaviour completely (25) (26). An example of this is a student who keeps receiving bad grades on their exam despite studying for hours. Over time, the individual will reduce the amount of time they are studying, thus continuing to earn poor grades.
Sociocultural
In the sociocultural theory, the role of family and one’s social environment play a substantial role in the development of depressive disorders. There are two sociocultural views- the family-social perspective and the multi-cultural perspective.
Family-social perspective. Similar to that of the behavioural theory, the family-social perspective of depression suggests that depression is related to the unavailability of social support. This is often supported by research studies that show separated and divorced individuals are three times more likely to experience depressive symptoms than those that are married or even widowed (27). While many factors lead a couple to separate or end their marriage, some relationships end due to a spouse’s mental health issues, particularly depressive symptoms. Depressive symptoms have been positively related to increased interpersonal conflicts, reduced communication, and intimacy issues, all of which are often reported as causal factors leading to a divorce (28).
The family-social perspective can also be viewed oppositely, with stress and marital discord leading to increased rates of depression in one or both spouses (29). While some research indicates that having children provides a positive influence on one’s life, it can also lead to stress both within the individual, as well as between partners due to division of work and discipline differences. Studies have shown that women who had three or more young children and also lacked a close confidante and outside employment, were more likely than other mothers to become depressed (30).
Multi-cultural perspective. While depression is experienced across the entire world, one’s cultural background may influence what symptoms of depression are presented. Common depressive symptoms such as feeling sad, lack of energy, anhedonia, difficulty concentrating, and thoughts of suicide are a hallmark in most societies; other symptoms may be more specific to one’s nationality. More specifically, individuals from non-Western countries (China and other Asian countries) often focus on the physical symptoms of depression—tiredness, weakness, sleep issues—and less emphasis on the cognitive symptoms. Individuals from
Within the United States (similar to Canada), many researchers have explored potential differences across ethnic or racial groups in both rates of depression, as well as presenting symptoms of those diagnosed with depression. These studies continually fail to identify any significant differences between ethnic and racial groups; however, one major study has identified a difference in the rate of recurrence of depression in Hispanic and African Americans (31). While the exact reason for this is unclear, researchers propose a lack of treatment opportunities as a possible explanation. According to Gonzalez and colleagues (31), approximately 54% of depressed white Americans seek out treatment, compared to the 34% and 40% Hispanic and African Americans, respectively. The fact that there is a large discrepancy in the use of treatment between white Americans and minority Americans suggests that these individuals are not receiving the effective treatment necessary to resolve the disorder, thus leaving them more vulnerable for repeated depressive episodes.
Gender differences. As previously discussed, there is a significant difference between gender and rates of depression, with women twice as likely to experience an episode of depression than men (32). There are a few speculations as to why there is such an imbalance in the rate of depression across genders.
The first theory, artifact theory, suggests that the difference between genders is due to clinician or diagnostic systems being more sensitive to diagnosing women with depression than men. While women are often thought to be more “emotional,” easily expressing their feelings and more willing to discuss their symptoms with clinicians and physicians, men often withhold their symptoms or will present with more traditionally “masculine” symptoms of anger or aggression. While this theory is a possible explanation for the gender differences in the rate of depression, research has failed to support this theory, suggesting that men and women are equally likely to seek out treatment and discuss their depressive symptoms (33)(34)
The second theory, hormone theory, suggests that variations in hormone levels trigger depression in women more than men (35). While there is biological evidence supporting the changes in hormone levels during various phases of the menstrual cycle and their impact on women’s ability to integrate and process emotional information, research fails to support this theory as the reason for higher rates of depression in women (36).
The third theory, the life stress theory, suggests that women are more likely to experience chronic stressors than men, thus accounting for their higher rate of depression (37). Women face increased risk for poverty, lower employment opportunities, discrimination, and poorer quality of housing than men, all of which are strong predictors of depressive symptoms (38).
The fourth theory, the gender roles theory, suggests that social and or psychological factors related to traditional gender roles also influence the rate of depression in women. For example, men are often encouraged to develop personal autonomy, seek out activities that interest them, and display achievement-oriented goals; women are encouraged to empathize and care for others, often fostering an interdependent functioning, which may cause women to value the opinion of others more highly than their male counterparts do.
The final theory, rumination theory, suggests that women are more likely than men to ruminate, or intently focus, on their depressive symptoms, thus making them more vulnerable to developing depression at a clinical level (39). Several studies have supported this theory and shown that rumination of negative thoughts is positively related to an increase in depression symptoms (40).
While many theories try to explain the gender discrepancy in depressive episodes, no single theory has produced enough evidence to fully explain why women experience depression more than men. Due to the lack of evidence, gender differences in depression remain one of the most researched topics within the subject of depression, while simultaneously being the least understood phenomena within clinical psychology.
Key Takeaways
- In terms of biological explanations for depressive disorders, there is evidence that rates of depression are higher among identical twins (the same is true for bipolar disorders), that the 5-HTT gene on chromosome 17 may be involved in depressive disorders, that norepinephrine and serotonin affect depressive (both being low) and bipolar disorders (low serotonin and high norepinephrine), the hormones cortisol and melatonin affect depression, and several brain structures are implicated in depression (prefrontal cortex, hippocampus, and amygdala) and bipolar disorder (basal ganglia and cerebellum).
- In terms of cognitive explanations, learned helplessness, attributional style, and maladaptive attitudes to include the cognitive triad, errors in thinking, and automatic thoughts, help to explain depressive disorders.
- Behavioural explanations centre on changes in the rewards and punishments received throughout life.
- Sociocultural explanations include the family-social perspective and multi-cultural perspective.
- Women are twice as likely to experience depression and this could be due to women being more likely to be diagnosed than men (called the artifact theory), variations in hormone levels in women (hormone theory), women being more likely to experience chronic stressors (life stress theory), the fostering of an interdependent functioning in women (gender roles theory), and that women are more likely to intently focus on their symptoms (rumination theory).
Review Questions
- How do twin studies explain the biological causes of mood disorders?
- What brain structures are implicated in the development of mood disorders? Discuss their role.
- What is learned helplessness? How has this concept been used to study the development and maintenance of mood disorders?
- What is cognitive triad?
- What are common cognitive distortions observed in individuals with mood disorders?
- What are the identified theories that are used to explain the gender differences in mood disorder development?
TREATMENT OF MOOD DISORDERS
Treatment of Mood Disorders Learning Objectives
- Describe treatment options for depressive disorders.
- Describe treatment options for bipolar disorders.
- Determine the efficacy of treatment options for depressive disorders.
- Determine the efficacy of treatment options for bipolar disorders.
Depressive Disorders
Given that Major Depressive Disorder is among the most frequent and debilitating psychiatric disorders, it should not be surprising that the research on this disorder is quite extensive. Among its treatment options, the most efficacious treatments include antidepressant medications, Cognitive-Behavioral Therapy (41), Behavioral Activation (42), and Interpersonal Therapy (43). Although CBT is the most widely known and used treatment for Major Depressive Disorder, there is minimal evidence to support one treatment modality over the other; treatment is generally dictated by therapist competence, availability, and patient preference (44).
Psychopharmacology – Antidepressant medications. Antidepressants are often the most common first-line attempt at treatment for MDD for a few reasons. Oftentimes an individual will present with symptoms to their primary caregiver (a medical doctor) who will prescribe them some line of antidepressant medication. Medication is often seen as an “easier” treatment for depression as the individual can take the medication at their home, rather than attending weekly therapy sessions; however, this also leaves room for adherence issues as a large percentage of individuals to fail to take prescription medication as indicated by their physician. Given the biological functions of neurotransmitters and their involvement in maintaining depressive symptoms, it makes sense that this is an effective type of treatment.
Within antidepressant medications, there are a few different classes, each categorized by its structural or functional relationships. It should be noted that no specific antidepressant medication class or medication has been proven to be more effective in treating MDD than others (APA, 2010). In fact, many patients may try several different types of antidepressant medications until they find one that is effective, with minimal side effects.
Psychopharmacology – Selective serotonin reuptake inhibitors(SSRIs). SSRIs are among the most common medications used to treat depression due to their relatively benign side effects. Additionally, the required dose to reach therapeutic levels is low compared to the other medication options. Possible side effects from SSRIs include but are not limited to nausea, insomnia, and reduced sex drive.
SSRIs improve depression symptoms by blocking the reuptake of norepinephrine and/or serotonin in presynaptic neurons, thus allowing more of these neurotransmitters to be available for postsynaptic neurons. While this is the general mechanism through which all SSRIs work, there are minor biological differences among different types of medications within the SSRI family. These small differences are actually beneficial to patients in that there are a few treatment options to maximize medication benefits and minimize side effects.
Psychopharmacology – Tricyclic antidepressants. Although originally developed to treat schizophrenia, tricyclic antidepressants were adapted to treat depression after failing to manage symptoms of schizophrenia (45). The term tricyclic came from the molecular shape of the structure: three rings.
Tricyclic antidepressants are similar to SSRIs in that they work by affecting brain chemistry, altering the number of neurotransmitters available for neurons. More specifically, they block the absorption or reuptake of serotonin and norepinephrine, thus increasing their availability for postsynaptic neurons. While effective, tricyclic antidepressants have been increasingly replaced by SSRIs due to their reduced side effects. However, tricyclic antidepressants have been shown to be more effective in treating depressive symptoms in individuals who have not been able to achieve symptom reduction via other pharmacological approaches.
While the majority of the side effects are minimal- dry mouth, blurry vision, constipation, others can be serious- sexual dysfunction, tachycardia, cognitive and/or memory impairment, to name a few. Due to the potential impact on the heart, tricyclic antidepressants should not be used in cardiac patients as they may exacerbate cardiac arrhythmias (46).
Psychopharmacology – Monoamine oxidase inhibitors (MAOIs). The use of MAOIs as a treatment for depression began serendipitously as patients in the early 1950s reported reduced depression symptoms while on the medication to treat tuberculosis. Research studies confirmed that MAOIs were effective in treating depression in adults outside the treatment of tuberculosis. Although still prescribed, they are not typically first-line medications due to their safety concerns with hypertensive crises. Because of this, individuals on MAOIs have strict diet restrictions to reduce their risk of hypertensive crises (47).
How do MAOIs work? In basic terms, monoamine oxidase is released in the brain to remove excess neurotransmitters norepinephrine, serotonin, and dopamine. MAOIs essentially prevent the monoamine oxidase (hence the name monoamine oxidase inhibitors) from removing these neurotransmitters, thus resulting in an increase in these brain chemicals (47). As previously discussed, norepinephrine, serotonin, and dopamine are all involved in the biological mechanisms of maintaining depressive symptoms.
While these drugs are effective, they come with serious side effects. In addition to the hypertensive episodes, they can also cause nausea, headaches, drowsiness, involuntary muscle jerks, reduced sexual desire, weight gain, etc. (APA, 2010). Despite these side effects, studies have shown that individuals prescribed MAOIs for depression have a treatment response rate of 50-70% (48). Overall, despite their effectiveness, MAOIs are likely the best treatment for late-stage, treatment-resistant depression patients who have exhausted other treatment options (48).
It should be noted that occasionally, antipsychotic medications are used for individuals with MDD; however, these are limited to individuals presenting with psychotic features.
Psychotherapy – Cognitive behavioural therapy (CBT). CBT was founded by Aaron Beck in the 1960s and is a widely practiced therapeutic tool used to treat depression (and other disorders as well). The basics of CBT involve what Beck called the cognitive triangle — cognitions (thoughts), behaviours, and emotions. Beck believed that these three components are interconnected, and therefore, affect one another. It is believed that CBT can improve emotions in depressed patients by changing both cognitions (thoughts) and behaviours, which in return enhances mood. Common cognitive interventions with CBT include thought monitoring and recording, identifying cognitive errors, examining evidence supporting/negating cognitions, and creating rational alternatives to maladaptive thought patterns. Behavioural interventions of CBT include activity planning, pleasant event scheduling, task assignments, and coping skills training.
CBT generally follows four phases of treatment:
- Phase 1: Increasing pleasurable activities. Similar to behavioUral activation (see below), the clinician encourages the patient to identify and engage in activities that are pleasurable to the individual. The clinician can help the patient to select the activity, as well as help them plan when they will engage in that activity.
- Phase 2: Challenging automatic thoughts. During this stage, the clinician provides psychoeducation about the negative automatic thoughts that can maintain depressive symptoms. The patient will learn to identify these thoughts on their own during the week and maintain a thought journal of these cognitions to review with the clinician in session.
- Phase 3: Identifying negative thoughts. Once the individual is consistently able to identify these negative thoughts on a daily basis, the clinician can help the patient identify how these thoughts are maintaining their depressive symptoms. It is at this point that the patient begins to have direct insight as to how their cognitions contribute to their disorder.
- Phase 4: Changing thoughts. The final stage of treatment involves challenging the negative thoughts the patient has been identifying in the last two phases of treatment and replacing them with positive thoughts.
Psychotherapy – Behavioural activation (BA). BA is similar to the behavioUral component of CBT in that the goal of treatment is to alleviate depression and prevent future relapse by changing an individual’s behaviour. Founded by Ferster (49), as well as Lewinsohn and colleagues (50)(51), the goal of BA is to increase the frequency of behavioUrs so that individuals have opportunities to experience greater contact with sources of reward in their lives. To do this, the clinician assists the patient by developing a list of pleasurable activities that they can engage in outside of treatment (i.e., going for a walk, going shopping, having dinner with a friend). Additionally, the clinician assists the patient in identifying their negative behaviours—crying, sleeping in, avoiding friends—and monitoring them so that they do not impact the outcome of their pleasurable activities. Finally, the clinician works with the patient on effective social skills. By minimizing negative behaviours and maximizing pleasurable activities, the individual will receive more positive rewards and reinforcement from others and their environment, thus improving their overall mood.
Psychotherapy – Interpersonal therapy (IPT). IPT was developed by Klerman, Weissman, and colleagues in the 1970s as a treatment arm for a pharmacotherapy study of depression (52). The treatment was created based on data from post-World War II individuals who expressed a substantial impact on their psychosocial life events. Klerman and colleagues noticed a significant relationship between the development of depression and complicated bereavement, role disputes, role transitions, and interpersonal deficits in these individuals (52). The idea behind IPT is that depressive episodes compromise interpersonal functioning, which makes it difficult to manage stressful life events. The basic mechanism of IPT is to establish effective strategies to manage interpersonal issues, which in return, will ameliorate depressive symptoms.
There are two main principles of IPT. First, depression is a common medical illness with a complex and multi-determined etiology. Since depression is a medical illness, it is also treatable and not the patient’s fault. Second, depression is connected to a current or recent life event. The goal of IPT is to identify the interpersonal problem that is related to the depressive symptoms and solve this crisis so the patient can improve their life situation while relieving depressive symptoms.
Multimodal treatment. While both pharmacological and psychological treatment alone is very effective in treating depression, a combination of the two treatments may offer additional benefits, particularly in the maintenance of wellness. Additionally, multimodal treatment options may be helpful for individuals who have not achieved wellness in a single modality.
Multimodal treatments can be offered in three different ways: concurrently, sequentially, or within a stepped manner (53). With a stepped manner treatment, pharmacological therapy is often used initially to treat depressive symptoms. Once the patient reports some relief in symptoms, psychosocial treatment is added to address the remaining symptoms. While all three methods are effective in managing depressive symptoms, matching patients to their treatment preferences may produce better outcomes than clinician-driven treatment decisions.
Bipolar Disorder
Psychopharmacology. Unlike treatment for MDD, there is some controversy regarding the effective treatment of Bipolar Disorder. One suggestion is to treat Bipolar Disorder aggressively with mood stabilizers such as Lithium or Depakote as these medications do not induce pharmacological mania/hypomania. These mood stabilizers are occasionally combined with antidepressants later in treatment only if absolutely necessary (54). Research has shown that mood stabilizers are less potent in treating depressive symptoms, and therefore, the combination approach is believed to help manage both manic and depressive episodes (54).
The other treatment option is to forgo the mood stabilizer and treat symptoms with newer antidepressants early in treatment. Unfortunately, large-scale research studies have not shown great support for this method (55)(56). Antidepressants often trigger a manic or hypomanic episode in bipolar patients. Because of this, the first-line treatment option for Bipolar Disorder is mood stabilizers, particularly Lithium.
Psychological treatment. Although psychopharmacology is the first and most widely used treatment for bipolar disorders, occasionally psychological interventions are also paired with medication as psychotherapy alone is not a sufficient treatment option. The majority of psychological interventions are aimed at medication adherence, as many bipolar patients stop taking their mood stabilizers when they “feel better” (57). Social skills training and problem-solving skills are also helpful techniques to address in the therapeutic setting as individuals with bipolar disorder often struggle in this area.
Outcome of Treatment
Depressive treatment. As we have discussed, the major depressive disorder has a variety of treatment options, all found to be efficacious. However, research suggests that while psychopharmacological interventions are more effective in rapidly reducing symptoms, psychotherapy, or even a combined treatment approach, are more effective in establishing long-term relief of symptoms.
Rates of relapse for major depressive disorder are often associated with individuals whose onset was at a younger age (particularly adolescents), those who have already experienced multiple major depressive episodes, and those with more severe symptomology, especially those presenting with severe suicidal ideation and psychotic features (APA, 2022).
Bipolar treatment. Lithium and other mood stabilizers are very effective in managing symptoms of patients with bipolar disorder. Unfortunately, it is the adherence to the medication regimen that is often the issue with these patients. Bipolar patients often desire the euphoric highs that are associated with manic and hypomanic episodes, leading them to forgo their medication. A combination of psychopharmacology and psychotherapy aimed at increasing the rate of adherence to medical treatment may be the most effective treatment option for bipolar I and II disorder.
Key Takeaways
You should have learned the following in this section:
- Treatment of depressive disorders includes psychopharmacological options such as anti-depressant mediations, SSRIs, tricyclic antidepressants, and MAOIs AND/OR psychotherapy options including CBT, behavioural activation (BA), and interpersonal therapy (IPT). A combination of the two main approaches often works best, especially in relation to the maintenance of wellness.
- Treatment of bipolar disorder involves mood stabilizers such as Lithium and psychological interventions with the goal of medication adherence, as well as social skills training and problem-solving skills.
- In regard to depression, psychopharmacological interventions are more effective in rapidly reducing symptoms, while psychotherapy, or even a combined treatment approach, is more effective in establishing long-term relief of symptoms.
- A combination of psychopharmacology and psychotherapy aimed at increasing the rate of adherence to medical treatment may be the most effective treatment option for bipolar I and II disorder.
Module Recap
That concludes our discussion of mood disorders. You should now have a good understanding of the two major types of mood disorders – depressive and bipolar disorders. Be sure you are clear on what makes them different from one another in terms of their clinical presentation, epidemiology, comorbidity, and etiology. This will help you with understanding treatment options and their efficacy.
Attribution
“Mood Disorders” by Washington State University is licensed under CC BY-NC-SA 4.0 (3rd edition as of August 2022)
References:
APA (2022) Association, A. P. (2022). Desk Reference to the Diagnostic Criteria from DSM-5-TR(tm). American Psychiatric Publishing.
- APA, 2022, pg. 139
- APA, 2022, pg. 177
- Daffin, K. M. a. B. a. L. (n.d.). Behavioral Disorders of Childhood – Simple Book Publishing. Pressbooks. https://opentext.wsu.edu/behavioral-disorders-childhood/
- Chen, L., Zhang, G., M., & Liang, X. (2013) Eye movement desensitization and reprocessing versus cognitive-behavioural therapy for adult posttraumatic stress disorder: Systematic review and meta-analysis Journal of Nervous & Mental Disease, 203, 443-451.
- Nolen-Hoeksema, S. (2001) Gender differences in depression. Current Directions in Psychological Research, 10, 173-176
- Bauer, M. & Pfenning, A. (2005). Epidemiology of Bipolar Disorders. Official Journal of the International League Against Epilepsy, 46, 8-13.
- Kessler, R., Berguland, P., Demler, O.,, Jin, R., Merikangas, K., . . . Wang, P, (2003 Results from the national comorbidity survey replication (NCS-R). Journal of American Medical Association, 289(23), 3095-3105
- Gotlib, I. & Hammen, C. (2009). Handbook of Depression, 2nd ed. New York, NY: Guildford Press
- Levinson, D. & Nichols, W. (2014). Major Depression and genetics. Stanford, A: Stanford, School of Medicine
- McGuffin, P., Katz, R., Watkins, S., & Rutherford, J. (1996). A hospital-based twin register of the heritability of DSM-IV unipolar depression. Archives of General Psychiatry, 53, 129- 136.
- Jansen, R., Penninx, B., Madar, V., Xia, K., Milaneschi, Y., Hottenga, J., . . . Sullivan, P. (2016). Gene expression in major depressive disorder. Molecular Psychiatry, 21, 339-347.
- Edvardsen, J., Torgersen, S., Roysamb, E., Lygren, S., Skre, I., Onstad, S., & Oien, P. (2008). Heritability of bipolar spectrum disorders. Unity or heterogeneity. Journal of Affective Disorders, 106(3), 229-240
- Ayd, F. (1956). A clinical evaluation of Frenquel. Journal of Nervous and Mental Disease, 124, 507-509.
- Ding, Y., Naganawa, M., Gallezot, J., Nabulsi, N., Lin, S., Ropchan, J., Weinzimmer, D., . . .
Laurelle, M. (2014). Clinical doses of atomozetime significantly occupy both norepinephrine and serotonin transports: Implications on treatment of depression and ADHD. Neuroimage, 86, 164-171 - Soreff, S., & McInnes, L., (2014). Bipolar affective disorder. Retrieved from http://emedicine.medscape.com/article/286342-overview.
- Owens, M., Herbert, J., Jones, P., Shakian, A., Wilkinson, P., Dunn, V., . . . Stuart, G. (2014). Elevated morning cortisol is a stratified population-level biomarker for major depression in boys only with high depressive symptoms. Proceedings of the National Academy of Sciences of the United States of America, 111(9), 3638-3643.
- Houenou, J., Frommberger, J., Carde, S., Glasbrenner, M., Diener, C., Leboyer, M. & Wessa, M. (2011). Neuroimaging-based markers of bipolar disorder: Evidence from two meta- analyses. Journal of Affective Disorders, 132(3), 344-355
- Seligman, M. (1975). Helplessness. San Francisco: Freeman.
- Nolen-Hoeksema, S., Girgus, J., & Seligman, M.(1992). Predictors and consequences of childhood depressive symptoms: A 5-year longitudinal study. Journal of Abnormal Psychology, 101(3), 405-422
- Beck, A. (2002). Cognitive models of depression. In R. L. Leahy & E.T. Dowd (Eds). Clinical advance sin cognitive psychotherapy: Theory and application (pp. 29-61). New York: Springer.
- Beck, A. (1991). Cognitive therapy: A 30-year retrospective, American Psychologist, 46(4), 368- 375.
- Beck, A. (1967). Depression: Causes and treatment. Philadelphia: University of Pennsylvania Press.
- ai, C., Zauszniewski, J., Tang, T., Hou, S., Su, S., & Lai, P. (2014). Personal beliefs, learned resourcefulness, and adaptive functioning in depressed adults. Journal of Psychiatric and Mental Health Nursing, 21(3), 280-287.
- Possel, P. & Black, S. (2014). Testing three different sequential mediational interpretations of Beck’s cognitive model of the development of depression. Journal of Clinical Psychology, 70(1), 72-94.
- Lewinsohn, P., Clarke, G., Hops, H., & Andrews, J. (1990). Cognitive-behavioral treatment for depressed adolescents. Behavior Therapist, 21, 385-401
- Lewinsohn, P., Antonuccio, D., Steinmetz, J. & Teri, L. (1984). The coping with depression course. Eugene, OR: Castalia.
- Schultz, G. (2007). Marital breakdown and divorce increases rates of depression, Stat-Can study finds. LifeSiteNews.com
- Najman, J., Khatun, M., Mamun, A., Clavarino, A., Williams, G., Scott, J., . . . Alati, R. (2014). Does depression experienced by mothers lead to a decline in marital quality: A 21-year longitudinal study. Social Psychiatry and Psychiatric Epidemiology, 49, 121-132.
- Nezlek, J., Hampton, C. & Shean, G. (2000). Clinical depression and day-to-day social interaction in a community sample. Journal of Abnormal Psychology, 109, 11-19.
- Brown, A. S., Begg, M. D., Gravenstein, S., Schaefer, C. A., Wyatt, R. J., Bresnahan, M., … & Susser, E. S. (2004). Serologic evidence of prenatal influenza in the etiology of schizophrenia. Archives of general psychiatry, 61(8), 774-780.
- Gonzalez, H., Tarraf, W., Whitfield, K., & Vega, W. (2010). The epidemiology of major depression and ethnicity in the United States. Journal of Psychiatric Research, 44, 1043- 1051.
- Schuch, J., Roest, A., Nolen, W., Penninx, B., & de Jonge, P. (2014). Gender difference in major depressive disorder: Results from the Netherlands study of depression and anxiety. journal of Affective Disorders, 156, 156-163.
- McSweeny, S. (2004). Depression in women. In L. Cosgrove & P.J. Caplan (Eds.), Bias in
psychiatric diagnosis (pp. 183-188). Northvale, NJ: Jason Aronson. - Rieker, P. & Bird, C. (2005). Rethinking gender differences in health: What we need to integrate social and biological perspectives. Journal of Gerontology, 60, S40-S47.
- Graziottin, A. & Serafini, A. (2009). Depression and the menopause: Why antidepressants are not enough? Menopause International, 15, 76-81
- Whiffen, V. & Demidenko, N. (2006). Mood disturbance across the life span. In J. Worell & C. D. Goodheart (Eds.), Handbook of girls’ and women’s psychological health (pp 51-59). New York: Oxford University Press
- Astburry, J. (2010). The social causes of women’s depression: A question of rights violated? In D.C., Jack & A. Ali (Eds.), Silencing the self across cultures: Depression and gender in the social world (pp. 19-45). New York: Oxford University Press.
- Garcia-Toro, M., Rubio, J., Gili, M., Roca, M., Jin, C., Liu, S., . . . Blanco, C. (2013). Persistence of chronic major depression: A national prospective study. Journal of Affective Disorders, 151, 306-312.
- Nolen-Hoeskema, S. (2012). Emotion regulation and psychopathology: The role of gender. Annual Review of Clinical Psychology, 8, 161-187.
- Hankin, B. (2009). Development of sex differences in depressive and co-occurring anxious symptoms during adolescence: Descriptive trajectories and potential explanations in a multiwave prospective study. Journal of Clinical Child and Adolescent Psychology, 38, 460-472.
- Beck, A. (1991). Cognitive therapy: A 30-year retrospective, American Psychologist, 46(4), 368- 375.
- Jacobson, N., Martell, C., & Dimidjian, S. (2001). Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology Science and Practice, 8(3), 255-270.
- Klerman, G., Weissman, M., Rounsaville, B., & Chevron, E. (1984). Interpersonal psychotherapy of depression. London: Jason Aronson Inc.
- Craighhead, E., & Dunlop, B. (2014). Combination psychotherapy and antidepressant medication treatment for depression: For whom, when, and how. Annual Review of Psychology, 65, 267-300
- Kuhn, R. (1958). The treatment of depressive states with G-22355 (imipramine hydrochloride). American Journal of Psychiatry, 115, 459-464
- Roose, S., & Spatz, E. (1999). Treating depression in patients with ischemic heart disease. Drug Safety, 20, 459-465
- Shulman, K., Herrmann, N., & Walker, S. (2013). Current place of monamine oxidase inhibitors in the treatment of depression. CNS Drugs, 27, 789-797
- Krishan, K. (2007). Revisiting monamine oxidase inibitors. Journal of Clinical Psychiatry, 68, 35-41.
- Ferster, C. (1973). A functional analysis of depression. American Psychologist, 28(10), 857-870.
- Lewinsohn, P. (1974). A behavioral approach to depression. In R. M. Freidman & M. M. Katz (Eds.), The psychology of depression: Contemporary theory and research (pp. 157-185). New York: Wiley.
- Lewinsohn, P., Biglan, A., & Zeiss, A. (1976). Behavioral treatment of depression. In P. O. Davidson (Ed), The behavioral management of anxiety, depression and pain (pp. 91- 146). New York: Brunner/Mazel.
- Klerman, G., Weissman, M., Rounsaville, B., & Chevron, E. (1984). Interpersonal psychotherapy of depression. London: Jason Aronson Inc.
- McGorry, P., Nelson, B., Goldstone, S., & Yung, A. (2010). Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Canadian Journal of Psychiatry, 55, 486-496.
- Nivoli, A., Colom, F., Murru, A., Pacchiarotti, I., Castro-Loli, P., Gonzalez-Pinto, A., …Vieta, E.(2011) New treatment guidelines for acute bipolar depression: A systematic review. Journal of Affective Disorders, 129(1-3), 14-26(2011).
- Gijsman, H., Geddess, J., Rnedell, J., Nolen, W., Goodwin, G. (2004). Antidepressants for bipolar depression: a systematic review of randomized, controlled trials. American Journal of Psychiatry, 161, 1537-1547.
- Moller, H.J., Grunze, H., & Broich, K. (2006). Do recent efficacy data on the drug treatment of acute bipolar depression support the position that drugs other than antidepressants are the treatment of choice?: A conceptual review. European Archives of Psychiatry and Clinical Neuroscience, 256, 1-16.
- Advokat, C., Comaty, J., Julien, R. (2014). Julien’s primer of drug reaction. New York: Worth Publishers

