Physical Development in Middle Childhood
Chapter Objectives
After this chapter, you should be able to:
- Examine nutrition and its impact on development.
- Explore physical development at this stage of childhood.
- Describe physical activities that can be expected in middle childhood.
Introduction
Children in middle childhood go through tremendous changes in the growth and development of their brain. During this period of development children’s bodies are not only growing, but they are becoming more coordinated and physically capable. Children are more mindful of their greater abilities in school and are becoming more responsible for their health and diet.
For Child and Youth Care Practitioners (CYCPs) this information can support and encourage physical activity through our work with young people and families. We can plan activities and interventions that focus on physical development that is fun, age-appropriate, and has structured goals or objectives.
Brain development
The brain reaches its adult size at about age seven. Then between 10 and 12 years of age, the frontal lobes become more developed and improvements in logic, planning, and memory are evident (van der Molen & Molenaar, 1994, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). The school-aged child is better able to plan and coordinate activity using both the left and right hemispheres of the brain, which control the development of emotions, physical abilities, and intellectual capabilities. The attention span also improves as the prefrontal cortex matures. The myelin also continues to develop and the child’s reaction time improves as well. Myelination improvement is one factor responsible for these growths.
From age 6 to 12, the nerve cells in the association areas of the brain, that is those areas where sensory, motor, and intellectual functioning connect, become almost completely myelinated (Johnson, 2005, as cited in Paris et al., 2021). This myelination contributes to increases in information processing speed and the child’s reaction time. The hippocampus, which is responsible for transferring information from the short-term to long-term memory, also shows increases in myelination resulting in improvements in memory functioning (Rolls, 2000, as cited in Paris et al., 2021).
Physical growth
Middle childhood spans the years between early childhood and adolescence, children are approximately 6 to 12 years old. While growth spurts can happen, in general physical growth rates are generally slow and steady during these years. (Spreen, Riser, & Edgell, 1995, as cited in Paris et al., 2021). Typically, a child will gain about 5-7 pounds a year and grow about 2 inches per year. They also tend to slim down and gain muscle strength. As bones lengthen and broaden and muscles strengthen, many children want to engage in strenuous physical activity and can participate for longer periods of time. In addition, the rate of growth for the extremities is faster than for the trunk, which results in more adult-like proportions. Long-bone growth stretches muscles and ligaments, which results in many children experiencing growing pains, at night, in particular.
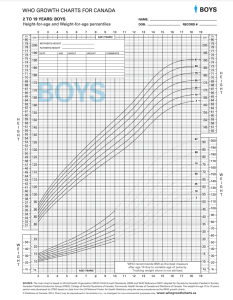
Figure 11.1: Dieticians of Canada (2014a)
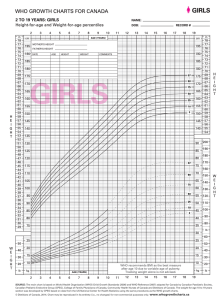
Figure 11.2: Dieticians of Canada (2014b).
As you can see from the above charts, there is a similarity in the average heights and weights of boys and girls during this developmental stage. For instance, at the age of 6 boys in the 50th percentile weigh 47 pounds and are 45.5 inches tall and girls measure in at 46 pounds and 45 inches tall. At the age of 9, boys in the 50th percentile weigh 52 pounds and are 62 inches tall and girls measure at the same. It also should be noted here that the World Health Organization (WHO; as cited in Pye, Scoffin, Quaid & Krieg, 2022) recommends Body Mass Index (BMI) as the best measure of weight after age 10, due to variable age of puberty and tracking weight alone is not advised (Dieticians of Canada, 2014b). According to the Childhood Obesity Foundation (n.d.), BMI is an indirect indicator of body fat. It is a measurement based on height and weight that tells if a child, or adult, is in a healthy range compared to his or her peers. It should be noted that BMI may not be an accurate indicator of body fat if your child is very muscular.
Beyond height and weight, a child’s physical growth can be seen in other ways. Children between ages 6 and 12, show significant improvement in their abilities to perform physical motor skills. This development growth allows children to gain greater control over the movement of their bodies, mastering many gross motor skills that were beyond that of the younger child. The Continuum of Development shares that during these middle childhood years, the development of gross motor skills continues to focus on increasing coordination, speed, and endurance (Ontario Ministry of Education, 2014).
Specifically, the gross motor skills that we see strengthen most, in children aged 6-12, are:
- Running: increasing control, speed and coordination;
- Jumping: jumping vertically increases in height, standing broad jump increases in length;
- Throwing: throwing speed, distance and accuracy improve;
- Catching: catching small balls over greater distances;
- Kicking: kicking speed and accuracy improve.
(Ontario Ministry of Education, 2014)
Physical activity at this age is an important factor for healthy development. Being active – as well as being sedentary (or inactive) can both impact children. Sedentary behaviour “means time spent doing very little physical activity, such as sitting at a computer, playing video games, or watching television” (Caring for Kids, 2018).
The benefits of an active, healthy lifestyle for kids, according to Caring for Kids (2018) means they can:
- keep their heart and lungs strong and healthy,
- become more flexible,
- develop strong bones,
- keep a healthy body weight,
- lower the risk of several diseases and health problems,
- improve their mood and self-esteem, and
- do better in school.
ParticipAction (2021) in partnership with the Government of Canada and other health organizations have developed the ’24-Hour Movement Guidelines’ which describe activity and sleep guidelines for every age. For children in middle childhood, the recommendations are for “at least 60 minutes per day of moderate to vigorous physical activity involving a variety of aerobic activities. Vigorous physical activities and muscle and bone strengthening activities should each be incorporated at least 3 days per week” (ParticipAction, 2021 p. 2). The guidelines also recommend nine to 11 hours of sleep for children ages 5-13, and no more than 2 hours of non-school related screen time per day (ParticipAction, 2021).
There are countless resources we as CYCPs can use to inform our choice of activities. Check out the list below to get you started!
Resources
The following are a short list to give us some ideas and a starting point:
Jumpstart – Canadian Tire Play Resources
Caring for Kids – Canadian Paediatric Society
Government of Canada – Children and physical activity
Nutritional needs
Let’s think for a moment about what our parents and grandparents used to eat? What are some of the differences that you may have experienced as a child?
Our diet has changed drastically as processed foods, which did not exist a century ago, and animal-based foods now account for a large percentage of our calories. Not only has what we eat changed, but the amount of it that we consume has greatly increased as well, as plates and portion sizes have grown much larger. All of these choices impact our health, with short- and long-term consequences as we age. Possible effects in the short-term include excess weight gain and constipation. The possible long-term effects, primarily related to obesity, include the risk of cardiovascular disease, diabetes, hypertension, as well as other health and emotional problems for children (Pye et al., 2022).
During middle childhood, a healthy diet facilitates physical, social/emotional and cognitive development and helps to maintain health and wellness. School-aged children experience steady, consistent growth, but at a slower rate than they did in early childhood. This slowed growth rate can have a lasting impact if nutritional, caloric, and activity levels aren’t adjusted in middle childhood which can lead to excessive weight gain early in life and can lead to obesity into adolescence and adulthood. Making sure that children have proper nutrients will allow for optimal growth and development.

Image 11.2: Government of Canada (2020)
The Government of Canada (2020), via their Canada Food Guide, recommends that individuals over the age of six:
- Eat plenty of vegetables and fruits, whole grain foods and protein foods. Choose protein foods that come from plants more often.
- Choose foods with healthy fats instead of saturated fat
- Limit highly processed foods. If you choose these foods, eat them less often and in small amounts.
- Prepare meals and snacks using ingredients that have little to no added sodium, sugars or saturated fat
- Choose healthier menu options when eating out
- Make water your drink of choice
- Replace sugary drinks with water
- Use food labels
- Be aware of food marketing
- Be mindful of eating habits (take time to eat; notice when full/hungry),
- Cook more often (plan what to eat; involve others in the preparation)
- Enjoy food
- Eat meals with others
One way to encourage children to eat healthy foods is to make meal and snack time fun and interesting. Parents should include children in food planning and preparation, for example selecting items while grocery shopping or helping to prepare part of a meal, such as making a salad. At this time, parents can also educate children about kitchen safety. It might be helpful to cut sandwiches, meats, or pancakes into small or interesting shapes. In addition, parents should offer nutritious desserts, such as fresh fruits, instead of calorie-laden cookies, cakes, salty snacks, and ice cream. Studies show that children who eat family meals on a frequent basis consume more nutritious foods.
As CYCPs, we often provide snacks or incorporate food in our work. For example, in residential programs, there are specific requirements that must be followed, informed by Canada’s Food Guide. In after school or community-based programs, snacks are usually found. We can encourage children and families to participate in the planning and preparation of food and snacks; there are many life skills that are present in food prep!
Energy
Children’s energy needs vary, depending on their growth and level of physical activity. Energy requirements also vary according to gender. Girls require 1,200 to 1,400 calories a day from age 2 to 8 and 1,400-1,800 for age 9 to 13. Boys also need 1,200 to 1,400 calories daily from age 4 to 8 but their daily caloric needs go up to 1,600-2,000 from age 9 to 13. This range represents individual differences, including how active the child is.
Recommended intakes of macronutrients (protein, carbohydrates, and fats) and most micronutrients (vitamins and minerals) are higher relative to body size, compared with nutrient needs during adulthood. Therefore, children should be provided nutrient-dense food at meal- and snack-time. However, it is important not to overfeed children, as this can lead to childhood obesity.
Malnutrition in children
Many may not know that malnutrition is a problem that many children face, in both developing nations and the developed world. Even with the wealth of food in North America, many children grow up malnourished, or even hungry. Household food insecurity is the inadequate or insecure access to food because of income or finances. It is a serious public health issue in Canada that that negatively impacts physical, mental, and social health, and costs our healthcare system considerably (Dieticians of Canada, 2021). In 2017-2018, one in eight Canadian households was food insecure, amounting to 4.4 million people, including 1.2 million children (PROOF, 2021).
Growing up in a food insecure environment can have significant consequences on a child’s healthy growth and development and well-being. According to Children First Canada (2020), food insecurity can affect children in the following ways:
- Obesity: Most caregivers ensure that their children are fed as much as possible, despite any financial setbacks, however these same parents may not have the money or time to prepare nutritious meals. This can lead to families eating a lot of cheap foods with low nutrition density (Government of Canada, 2019).
- Nutritional and vitamin deficiencies: Children eating foods that are not nutrient-dense can end up with various nutritional deficiencies leading to fatigue or even illness. Anemia, stunted growth or bone deformities and abnormalities may occur. Additionally, children who are nutrient-deficient will also be moodier and face more challenges maintaining emotional stability, which hinders their ability to mature in this area.
- School challenges: Children who don’t get sufficient nutrition are going to be fatigued throughout the day and this can impact their educational performance. They may end up with poor grades, even if they’ve done all of the required work and studying. They may have a harder time making friends and forming bonds, stunting their emotional and social development.
- Parental stress: Adults who are dealing with food and financial insecurity are likely to be stressed, depressed or otherwise unwell. Over-stressed caregivers aren’t able to give as much time and attention to their children and even with the best intentions, they may end up emotionally blocked off. When the parents are stressed, so are the children.
- Generational poverty: Children who grow up in food-insecure homes can easily turn into adults who lead food-insecure homes. While many people aspire to do better than the households that they came from, it’s harder to move up in life when you have fewer resources available to you.
This area of focus is key for us as CYCPs, as we can provide resources to families and incorporate this knowledge into our work – including our interventions, supports, and programming.
Indigenous Perspectives
This article First Nations Nutrition discusses the risk of malnourishment and chronic diseases in First Nations children.
Common Challenges with Physical Health
Vision and Hearing
The most common vision problem in middle childhood is being nearsighted, otherwise known as Myopic. 25% of children will be diagnosed by the end of middle childhood. Being nearsighted can be corrected by wearing glasses with corrective lenses.

Image 11.3: A child receiving an eye exam. (Image is in the public domain)
Children may have many ear infections in early childhood, but it’s not as common within the 6-12 year age range. Numerous ear infections during middle childhood may lead to headaches and migraines, which may result in hearing loss.
Oral Health
Children in middle childhood will start or continue to lose teeth. They experience the loss of deciduous, or “baby,” teeth and the arrival of permanent teeth, which typically begins at age six or seven, although it can start as early as the age of 4. It is important for children to continue seeing a dentist twice a year to be sure that these teeth are healthy.
The foods and nutrients that children consume are also important for dental health. Offer healthy foods and snacks to children and when children do eat sugary or sticky foods, they should brush their teeth afterward.
Image11.4: A boy brushing his teeth. (Image by Latrobebohs is licensed under CC BY-SA 3.0)
Children should floss daily and brush their teeth at least twice daily: in the morning, at bedtime, and preferably after meals. Parents or caregivers are encouraged to supervise brushing until your child is 7 or 8 years old to avoid tooth decay.
The best defence against tooth decay is flossing, brushing and adding fluoride; a mineral found in most tap water. If your water doesn’t have fluoride, ask a dentist about fluoride drops, gel or varnish. Also ask your child’s dentist about sealants—a simple, pain-free way to prevent tooth decay. These thin plastic coatings are painted on the chewing surfaces of permanent back teeth. They quickly harden to form a protective shield against germs and food. If a small cavity is accidentally covered by a sealant, the decay won’t spread because germs trapped inside are sealed off from their food supply.
Children’s dental health needs continuous monitoring as children lose teeth and new teeth come in. Many children have some malocclusion (when the way upper teeth aren’t correctly positioned slightly over the lower teeth, including under- and overbites) or malposition of their teeth, which can affect their ability to chew food, floss, and brush properly. Dentists may recommend that it’s time to see an orthodontist to maintain proper dental health. Dental health is exceedingly important as children grow more independent by making food choices and as they start to take over flossing and brushing. Parents can ease this transition by promoting healthy eating and proper dental hygiene.
In Ontario, children under the age of 17 years may be eligible for free dental care through the governments Healthy Smiles for low-income families (Government of Ontario, 2021).
Diabetes in Childhood
Until recently diabetes in children and adolescents was thought of almost exclusively as type 1, but that thinking has evolved. Type 1 diabetes is the most common form of diabetes in children and is the result of a lack or production of insulin due to an overactive immune system. Type 2 diabetes used to be referred to as adult-onset diabetes as it was not common during childhood. But with increasing rates of overweight and obesity in children and adolescents, more Type 2 diagnoses are happening before adulthood. It is also important to note that Type 2 disproportionately affects minority youth.

Image 11.5: The finger-prick blood sugar test for diabetes. (Image by the U.S. Army is in the public domain)
Asthma
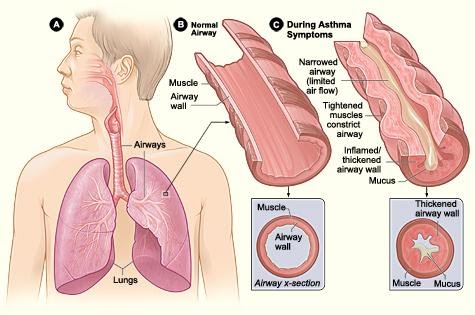
Childhood asthma that is unmanaged may make it difficult for children to develop to their fullest potential. Asthma is a chronic lung disease that inflames and narrows the airways. Asthma causes recurring periods of wheezing (a whistling sound when you breathe), chest tightness, shortness of breath, and coughing. The coughing often occurs at night or early in the morning. Asthma affects people of all ages, but it most often starts during childhood. According to Asthma Canada (n.d.), over 850,000 children under the age of 14 in Canada are affected by asthma. Asthma is the leading cause of school absences.
To understand asthma, it helps to know how the airways work. The airways are tubes that carry air into and out of your lungs. People who have asthma have inflamed airways. The inflammation makes the airways swollen and very sensitive. The airways tend to react strongly to certain inhaled substances. When the airways react, the muscles around them tighten. This narrows the airways, causing less air to flow into the lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways might make more mucus than usual. Mucus is a sticky, thick liquid that can further narrow the airways. This chain reaction can result in asthma symptoms. Symptoms can happen each time the airways are inflamed.
Sometimes asthma symptoms are mild and go away on their own or after minimal treatment with asthma medicine. Other times, symptoms continue to get worse. When symptoms get more intense and/or more symptoms occur, you’re having an asthma attack. Asthma attacks also are called flare-ups or exacerbations.
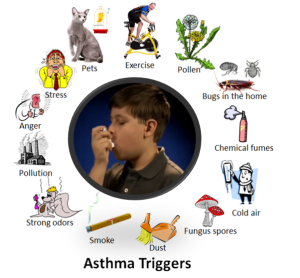
Treating symptoms when you first notice them is important. This will help prevent the symptoms from worsening and causing a severe asthma attack. Severe asthma attacks may require emergency care, and they can be fatal. Asthma has no cure. Even when you feel fine, you still have the disease and it can flare up at any time.
However, with today’s knowledge and treatments, most people who have asthma are able to manage the disease. They have few, if any, symptoms. They can live normal, active lives and sleep through the night without interruption from asthma. If you have asthma, you can take an active role in managing the disease. For successful, thorough, and ongoing treatment, build strong partnerships with your doctor and other health care providers (Pye et al., 2022).
Childhood stress
Take a moment to think about how you deal with and how stress affects you. Now think about what the impact of stress may have on a child and their development.
Children experience stress and different types of stressors differently. Not all stress is bad. Normal, everyday stress can provide an opportunity for young children to build coping skills and poses little risk to development. Even more long-lasting stressful events such as changing schools or losing a loved one can be managed fairly well. But children who experience toxic stress or who live in extremely stressful situations of abuse over long periods of time can suffer long-lasting effects. The structures in the midbrain or limbic system such as the hippocampus and amygdala can be vulnerable to prolonged stress during early childhood (Middlebrooks and Audage, 2008, as cited in Paris et al., 2021). High levels of the stress hormone cortisol can reduce the size of the hippocampus and effect the child’s memory abilities. Stress hormones can also reduce immunity to disease.
If the brain is exposed to long periods of severe stress it can develop a low threshold making the child hypersensitive to stress in the future.
Whatever the effects of stress, it can be minimized if a child learns to deal with stressors and develop coping strategies with the support of caring adults. It’s easy to know when your child has a fever or other physical symptoms. This is where CYCPs come in!
Summary
- Examining nutrition and its impact on development.
- Exploring physical development at this stage of childhood.
- Describing physical activities that can be expected in middle childhood.
References
Asthma Canada. (n.d.). Asthma at school. Retrieved from https://asthma.ca/get-help/asthma-in-children/asthma-at-school/
Caring for Kids. (2018). Physical activity for children and youth. Retrieved from https://caringforkids.cps.ca/handouts/healthy-living/physical_activity
Childhood Obesity Foundation. (n.d.). Is my child a healthy weight? Retrieved from https://childhoodobesityfoundation.ca/child-healthy-weight/
Children First Canada. (2020). 5 Eye-opening ways kids are affected by food insecurity. Retrieved from https://childrenfirstcanada.org/blog/5-eye-opening-ways-kids-are-affected-by-food-insecurity/
Dieticians of Canada. (2021). Dieticians take action on household food insecurity. Retrieved from https://www.dietitians.ca/foodinsecurity
Dieticians of Canada. (2014a). WHO growth charts for Canada: Boys. Retrieved from https://www.dietitians.ca/DietitiansOfCanada/media/Documents/WHO%20Growth%20Charts/Set-2-HFA-WFA_2-19_BOYS_SET-2_EN.pdf
Dieticians of Canada. (2014b). WHO growth charts for Canada: Girls. Retrieved from https://www.dietitians.ca/DietitiansOfCanada/media/Documents/WHO%20Growth%20Charts/Set-2-HFA-WFA_2-19_GIRLS_SET-2_EN.pdf
Encyclopedia on early childhood development. (2022-2023). Physical activity. Retrieved from https://www.child-encyclopedia.com/physical-activity
Government of Canada. (2020). Canada food guide: Healthy food choices. Retrieved from https://food-guide.canada.ca/en/healthy-food-choices/
Government of Canada. (2019). Childhood obesity. Retrieved from https://www.canada.ca/en/public-health/services/childhood-obesity/childhood-obesity.html
Government of Canada. (2016). Children and physical activity. Retrieved from https://www.canada.ca/en/public-health/services/being-active/children-physical-activity.html
Government of Ontario. (2021). Services covered by Healthy Smiles Ontario. Retrieved from https://www.ontario.ca/page/services-covered-by-healthy-smiles-ontario
Jumpstart. (2023). Resources for parents. Retrieved from https://jumpstart.canadiantire.ca/pages/resources-for-parents
Ontario Ministry of Education. (2014). Excerpts from “ELECT”. Retrieved from https://www.dufferincounty.ca/sites/default/files/rtb/Excerpts-from-Early-Learning-for-Every-Child-Today.pdf
ParticipAction. (2021). 24 Hour movement guidelines: Children (5-11) and youth (12-18). Retrieved from https://csepguidelines.ca/guidelines/children-youth/
ParticipAction. (2021). Ability toolkit. Retrieved from https://www.participaction.com/wp-content/uploads/2022/07/the_ability_toolkit.pdf
PROOF. (2021). Household food insecurity in Canada. Retrieved from https://proof.utoronto.ca/food-insecurity/
Pye, T., Scoffin, S., Quade, J., & Krieg, J. (2022). Child Growth and Development Canadian Ed. Retrieved from https://ecampusontario.pressbooks.pub/childgrowthanddevelopment/
OER Attributions:
Content from this reading has been adapted from the following sources:
Child Growth and Development Canadian Ed (2022) by Tanya Pye; Susan Scoffin; Janice Quade; and Jane Krieg is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
Child Growth and Development by Paris, Ricardo, Rymond, and Johnson is shared under a CC BY license, except where otherwise noted.

