Sample B: Vital Sign Measurement (Nursing)
What is temperature?
Temperature refers to the degree of heat or cold in an object or a human body. In humans, the brain’s hypothalamus acts as the body’s thermostat and is responsible for regulating its temperature (OER #2). See Figure 2.1 of the hypothalamus.
The human body is constantly adapting to internal health states and environmental conditions, and the hypothalamus is programmed to tell the body to generate heat if the body temperature is low. For example, the hypothalamus can activate peripheral vasoconstriction and shivering (contraction of skeletal muscles) to prevent a decrease in body temperature. The hypothalamus can also reduce heat if the body temperature is too high. For example, it can activate peripheral vasodilation to increase heat loss and cause a person to perspire, which cools the body.
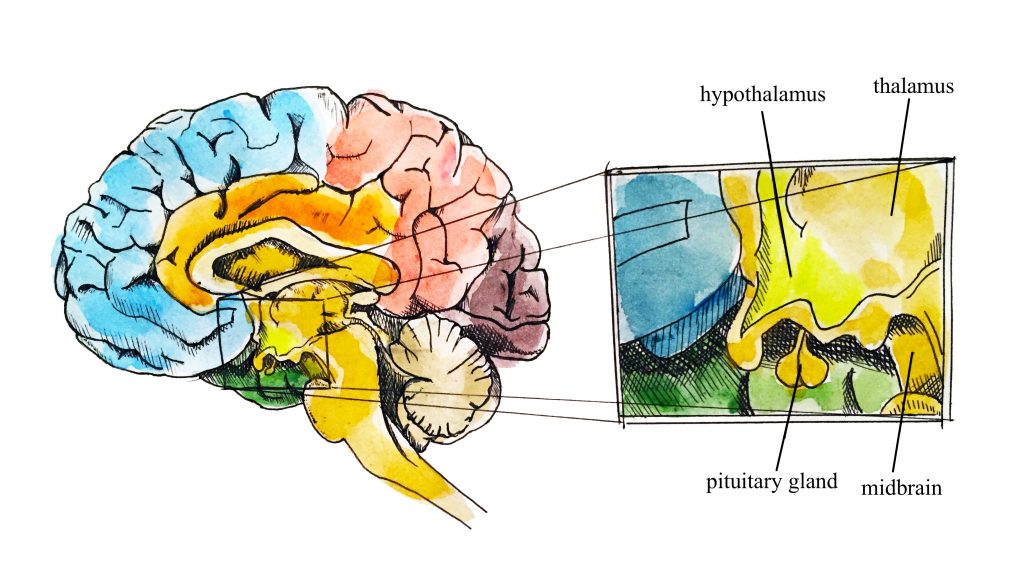
Figure 2.1: Hypothalamus (Illustration credit: Hilary Tang)
Why is temperature measured
Healthcare providers measure a client’s temperature because it can give information about their state of health and influence clinical decisions. Accurate measurements and interpretation are vital so that hyperthermia and hypothermia can be identified and appropriate interventions determined.
Hyperthermia refers to an elevated body temperature. It can be related to an internal or external source. External sources that increase body temperature could include exposure to excessive heat on a hot day or being in a sauna or hot tub. Internal sources that may increase body temperature include fever caused by an infection or tissue breakdown associated with physical trauma (e.g., surgery, myocardial infarction) or some neurological conditions (e.g., cerebral vascular accident, cerebral edema, brain tumour). Hyperthermia that is associated with an infectious agent, such as a bacteria or virus (e.g., the flu) is referred to as febrile. Unresolved hyperthermic body states can lead to cell damage.
Hypothermia refers to a lowered body temperature. It is usually related to an external source such as being exposed to the cold for an extended period of time. Hypothermia is sometimes purposefully induced during surgery, or for certain medical conditions, to reduce the body’s need for oxygen. Unresolved hypothermic body states can slow cellular processes and lead to loss of consciousness.
Methods of measurement
Methods of measuring a client’s body temperature vary based on developmental age, cognitive functioning, level of consciousness, state of health, safety, and agency/unit policy. The healthcare provider chooses the best method after considering client safety, accuracy, and least invasiveness, all contingent on the client’s health and illness state. The most accurate way to measure core body temperature is an invasive method through a pulmonary artery catheter. This is only performed in a critical care area when constant measurements are required along with other life-saving interventions.
Methods of measurement include oral, axillary, tympanic, rectal, temporal artery, and dermal routes.
Oral temperature can be taken with clients who can follow instructions, so this kind of measurement is common for clients over the age of four, or even younger children if they are cooperative. Another route other than oral (e.g., tympanic or axillary) is preferable when a client is on oxygen delivered via a face mask because this can alter the temperature.
For children younger than four, axillary temperature is commonly measured unless a more accurate reading is required.
Rectal temperature is an accurate way to measure body temperature (Mazerolle, Ganio, Casa, Vingren, & Klau, 2011). The rectal route is recommended by the Canadian Pediatric Society for children under two years of age (Leduc & Woods, 2017). However, this method is not used on infants younger than thirty days or premature infants because of the risk of rectal tearing. If the rectal method is required, the procedure is generally only used by nurses and physicians.
Temporal artery temperature is not a common method of measurement, but may be used in some agencies; this process involves holding the device and sliding it over the skin of the forehead and then, down over the temporal artery in one motion. Dermal strips can be placed on the forehead to measure skin temperature, but are not yet widely used, and the accuracy of this method has not yet been verified.
Points to consider
The accuracy of measurements is most often influenced by the healthcare provider’s adherence to the correct technique.
The following pages detail the normal temperature ranges and techniques associated with each of the temperature methods.
What are normal temperature ranges
The human body’s core temperature (internal body temperature) is measured in degrees Celsius (ºC) or Fahrenheit (ºF). In Canada, degrees Celsius is most commonly used.
In adults, the normal core body temperature (referred to as normothermia or afebrile) is 36.5–37.5ºC or 97.7–99.5ºF (OER #2).
A wider temperature range is acceptable in infants and young children, and can range from 35.5–37.7ºC or 95.9–99.8ºF. Infants and children have a wider temperature range because their heat control mechanisms are less effective. They are at risk for heat loss for many reasons including having less subcutaneous fat than adults, a larger body surface area in comparison to weight (and larger head size in proportion to the rest of the body), immature metabolic mechanisms (e.g., they may be unable to shiver), and limited ability to produce heat through activity. They are also at risk of excessive heat production due to crying and restlessness as well as external factors such as being wrapped in too many blankets.
Older adults tend to have lower body temperatures and are at risk for hypothermic states; reasons for this may include having less subcutaneous tissue acting as insulation, loss of peripheral vasoconstriction capacity, decreased cardiac output with resultant lowered blood flow to the extremities, decreased muscle mass resulting in reduced heat production capacity, and decreased metabolic responses.
Points to consider
It is important to monitor and regulate temperature in newborns and infants because of the temperature fluctuations that place them at higher risk for hypothermia and hyperthermia, whereas temperature changes in older adults are often minimal.
See Table 2.1 for normal temperature ranges based on method. The normal ranges vary slightly for each of the methods. As a healthcare provider, it is important to determine the significance of the temperature by considering influencing factors and the client’s overall state of health.
Table 2.1: Normal temperature ranges
| Method | Range |
|---|---|
| Oral | 35.8–37.3ºC |
| Axillary | 34.8–36.3ºC |
| Tympanic | 36.1–37.9ºC |
| Rectal | 36.8–38.2ºC |
Other factors that influence temperature include diurnal rhythm, exercise, stress, menstrual cycle, and pregnancy. The diurnal cycle causes a fluctuation of 1ºC, with temperatures lowest in the early morning and highest in the late afternoon. During exercise, body temperature rises because the body is using energy to power the muscles. Temperature can rise as a result of stress and anxiety, due to stimulation of the sympathetic nervous system and increased secretion of epinephrine and norepinephrine. Body temperature varies throughout a woman’s menstrual cycle due to hormonal fluctuations, rising after ovulation until menstruation by about 0.5–1ºC. Body temperature is slightly elevated during pregnancy as a result of increased metabolism and hormone production such as progesterone.
Oral temperature
The normal oral temperature is 35.8–37.3ºC (OER #1) or 96.4–99.1ºF. Oral temperature measurement is common and reliable because it is close to the sublingual artery. An oral thermometer is shown in Figure 2.2. The device has blue colouring, indicating that it is an oral or axillary thermometer as opposed to a rectal thermometer, which has red colouring.

Figure 2.2: Oral thermometer
Technique
Remove the probe from the device and place a probe cover (from the box) on the oral thermometer without touching the probe cover with your hands. Place the thermometer in the client’s mouth under the tongue and instruct client to keep mouth closed and not to bite on the thermometer (OER #1). Ensure the thermometer probe is in the posterior sublingual pocket under the tongue, slightly off-centre. Leave the thermometer in place for as long as is indicated by the device manufacturer (OER #1). The thermometer will beep within a few seconds when the temperature has been taken: most oral thermometers are electronic and provide a digital display of the reading. Discard the probe cover in the garbage (without touching the cover) and place the probe back into the device. See Figure 2.3 of an oral temperature being taken.

Figure 2.3: Oral temperature being taken
Technique tips
Putting the probe cover on takes practice. You need to ensure that it snaps onto the probe. Sometimes the device will turn off after you take the probe out of the device if you take too long to put the probe cover on or insert it in the client’s mouth. If so, discard the probe cover and re-insert the probe into the device to reset it. Then try again.
What should the healthcare provider consider?
Healthcare providers often measure the oral temperature, particularly when the client is conscious and can follow directions. However, certain factors can lead to an inaccurate oral temperature, including recent consumption of hot or cold food or a beverage, chewing gum, and smoking prior to measurement. Healthcare providers should wait up to 15 minutes to take the oral temperature if the client is eating hot or cold food or drinking a hot or cold beverage and about 5 minutes if the client is chewing gum or has just smoked. Alternatively, a different method is used to measure temperature. Measurement of the oral temperature is not recommended for individuals who are unconscious, unresponsive, confused, have an endotracheal tube secured in the mouth, and cannot follow instructions.
Tympanic temperature
The normal tympanic temperature is usually 0.3–0.6°C higher than an oral temperature (OER #1). It is accurate because the tympanic membrane shares the same vascular artery that perfuses the hypothalamus (OER #1). A tympanic thermometer is shown in Figure 2.4.

Figure 2.4: Tympanic thermometer
Technique
Remove the tympanic thermometer from the casing and place a probe cover (from the box) on the thermometer tip without touching the probe cover with your hands. Only touch the edge of the probe cover (if needed), to maintain clean technique. Turn the device on. Ask the client to keep head still. For an adult or older child, gently pull the helix up and back to visualize the ear canal. For an infant or younger child (under 3), gently pull the lobe down. The probe is inserted just inside the opening of the ear. Never force the thermometer into the ear and do not occlude the ear canal (OER #1). Only the tip of the probe is inserted in the opening – this is important to prevent damage to the ear canal. Activate the device; it will beep within a few seconds to signal it is done. Discard the probe cover in the garbage (without touching the cover) and place the device back into the holder. See Figure 2.5 of a tympanic temperature being taken.

Figure 2.5: Tympanic temperature being taken
Technique tips
The technique of pulling the helix up and back (adult) or the lobe down (child under 3) is used to straighten the ear canal so the light can reflect on the tympanic membrane. If this is not correctly done, the reading may not be accurate. The probe tip is gently inserted into the opening to prevent damage to the ear canal. The ear canal is a sensitive and a highly innervated part of the body, so it is important not to force the tympanic probe into the ear.
What should the healthcare provider consider?
The tympanic temperature method is a quick and minimally invasive way to take temperature. Although research has proven the accuracy of this method, some pediatric institutions prefer the accuracy of the rectal temperature. The Canadian Pediatric Society found equal evidence for and against the use of tympanic temperature route (Leduc & Woods, 2017). It concluded that tympanic temperature is one option for use with children, but suggested using rectal temperature for children younger than two, particularly when accuracy is vital. The tympanic temperature is not measured when a client has a suspected ear infection. It is important to check your agency policy regarding tympanic temperature.
Axillary temperature
The normal axillary temperature may be as much as 1ºC lower than the oral temperature (OER #1). An axillary thermometer is the same electronic device as an oral thermometer, and both have a blue end.
Technique
Remove the probe from the device and place a probe cover (from the box) on the thermometer without touching the cover with your hands. Ask the client to raise the arm away from his/her body. Place the thermometer in the client’s armpit (OER #1), on bare skin, as high up into the axilla as possible, with the point facing behind the client. Ask the client to lower his/her arm and leave the device in place for as long as is indicated by the device manufacturer (OER #1). Usually the device beeps in 10–20 seconds. Discard the probe cover in the garbage (without touching the cover) and place the probe back into the device. See Figure 2.6 of an axillary temperature being taken.

Figure 2.6: Axillary temperature being taken
What should the healthcare provider consider?
The axillary route is a minimally invasive way to measure temperature. It is commonly used in children. It is important to ensure that the thermometer is as high up in the axilla as possible with full skin contact and that the client’s arm is then lowered down.
Rectal temperature
The normal rectal temperature is usually 1ºC higher than oral temperature (OER #1). A rectal thermometer has a red end to distinguish it from an oral/axillary thermometer. A rectal thermometer is shown in Figure 2.7.

Figure 2.7: Rectal thermometer
Technique
First, ensure the client’s privacy. Wash your hands and put on gloves. For infants, lie them down in a supine position and raise their legs up toward the chest. You can encourage a parent to hold the infant to decrease movement and provide a sense of safety. With older children and adults, assist them into a side lying position. Remove the probe from the device and place a probe cover (from the box) on the thermometer. Lubricate the cover with a water-based lubricant, and then gently insert the probe 2–3 cm inside the rectal opening of an adult, or less depending on the size of the client. The device beeps when it is done.
What should the healthcare provider consider?
Measuring rectal temperature is an invasive method. Some suggest its use only when other methods are not available (OER #1), while others suggest that the rectal route is a gold standard in the infant population because of its accuracy. The Canadian Pediatric Society (Leduc & Woods, 2017) has referred to research indicating that rectal temperatures may remain elevated after a client’s core temperature has started to return to normal, but after reviewing all available evidence, still recommends measuring rectal temperature for children under the age of two, particularly when accuracy is vital. Rectal temperature is not measured in infants under one month of age or premature newborns.
Checking in
You have had to digest a fair bit of information in this chapter. Take a few moments to make sure your understand the different ways to take temperature and when to use the different methods.
Try it out: Oral temperature
Next, you have an opportunity to watch film clips on accurate measurement techniques. There are three activities that involve film clips that you can watch, and then try out yourself. Check it out!
Watch this short film clip 2.1 and see how oral temperature is taken correctly. After watching the clip, try the technique yourself. You can watch the clip and practice as many times as you like.
Film clip 2.1: Oral temperature
Try it out: Tympanic temperature
Watch this short film clip 2.2 and see how tympanic temperature is taken correctly. After watching the clip, try the technique yourself. You can watch the clip and practice as many times as you like.
Film clip 2.2: Tympanic temperature
Try it out: Axilla temperature
Watch this short film clip 2.3 and see how axilla temperature is taken correctly. After watching the clip, try the technique yourself. You can watch the clip and practice as many times as you like.
Film clip 2.3: Axilla temperature
Test yourself
Before you move to the next chapter, make sure you understand fully the content of this chapter. Your goal is to score 100% on each activity. Take as many attempts as you need.
Chapter summary
Temperature is an important vital sign because it provides current data about the client’s health and illness state. Changes in body temperature act as a cue for healthcare providers’ diagnostic reasoning.
There are many ways to measure temperature. In determining the best method, the healthcare provider considers agency policy, the client’s age and health and illness state, and the reason for taking the temperature. Healthcare providers must use the correct technique when measuring temperature, because this can influence client data.
When determining the relevance of the temperature, the healthcare provider considers the client’s baseline data and the situation. Diagnostic reasoning about temperature always involves considering additional data including other vital sign measurements and subjective and objective client data.
Part of this content was adapted from OER #2 (as noted in brackets above):
© Apr 10, 2017 OpenStax Anatomy and Physiology. Textbook content produced by OpenStax Anatomy and Physiology is licensed under a Creative Commons Attribution License 4.0 license. Download for free at http://cnx.org/contents/7c42370b-c3ad-48ac-9620-d15367b882c6@12
Main output of the limbic system. It is located on lower part of the top end of the brain stem.
Condition where an individual's body temperature is elevated beyond normal due to failed thermoregulation. The person's body produces or absorbs more heat than it dissipates.
Defined as a decrease in the core body temperature to at least 95 degrees F. It occurs when the heat loss is greater than the metabolic and heat production. Hypothermia can be categorized in three stages: mild, moderate and severe, based on core body temperature.
Once a day cycle
Endogenous steroid and progestogen sex hormone involved in the menstrual cycle, pregnancy, and embryogenesis of humans and other species. It belongs to a group of steroid hormones called the progestogens, and is the major progestogen in the body.
Prominent rim of the auricle
Space below the shoulder through which vessels and nerves enter and leave the upper arm; a person's armpit

