Phantom Pain
Incidence and Timing
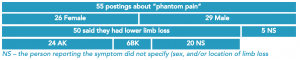
For the experience of phantom pain, the term “phantom pain” was used, which resulted in 55 responses.
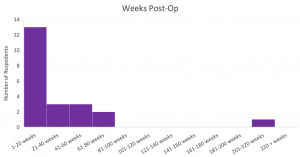
The duration of time since the osseointegration surgery was reported by 22 of the 55 respondents, with median time of 18 weeks post-surgery (range: 1 weeks – 208 weeks).
Symptoms
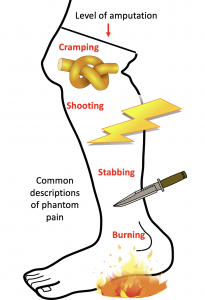
All of the respondents indicated that they experienced phantom pain since the surgery and described the pain in a variety of ways. There did not seem to be a correlation between type of pain experienced and duration of time since surgery. Further, responses were variable regarding phantom pain experience increasing or decreasing since surgery; some respondents stated they experienced aggravated phantom pain post-surgery, and some stated they experienced less painful phantom pain. One respondent described her phantom pain as being triggered by grinding in her prosthetic. A couple other respondents shared they had worse phantom pain after getting the Astra Zeneca vaccine for COVID-19, and another saying when they were sick with COVID-19 they had increased phantom pain. Descriptions of the phantom pain, while variable, tended to be more expressive than for other types of pain. Respondents used a multitude of powerful adjectives including stinging pain, burning pain, painful tingling, sharp pain, shocking pain, spasms of pain, and shooting pain. Many respondents also rated their phantom pain as intolerable when it happened and stated that it was the worst kind of pain they had experienced (some even rated their pain as 10/10 on the pain scale). This type of pain also seemed to be the hardest to gain relief from, with several respondents indicating that their episodes of pain lasted several hours (up to ten hours in one instance).
What People Have Tried
Respondents, to gain relief from the pain, used a variety of interventions. Most commonly used were pharmacological treatments that included ibuprofen, Cymbalta, Lyrica, gabapentin [1], oxycodone, tramadol, Targin, lorazepam, Flexeril, CBD oil, and Nummit cream. Some respondents also indicated that they took supplements, such as multivitamins, potassium, and vitamin B12, in an attempt to relieve pain. Mixed results were reported with medications, and no one medication seemed to work for everyone to relieve the phantom pain. Non-pharmacological treatments were listed as well by respondents and included reframing [2], mirror therapy [3], acupuncture [4], hypnotherapy, physiotherapy, transcutaneous electrical nerve stimulation, and shrinkers. Other treatments that were used were Epsom baths, ice baths, TMR, and reducing alcohol and caffeine intake. As with the medications listed above, variable results were reported with no one treatment providing definitive relief from phantom pain compared to others. Other respondents reported removing their prosthesis, walking with their prosthetic, distracting themselves, playing music, and wrapping their phantom leg in a blanket.
Fact Checkers
[1] According to a study by Molero et al. (2019), gabapentinoids (a drug class including gabapentin and pregabalin, brand name Lyrica) may cause in an increase in hazards of suicidal behaviour, unintentional overdoses, and head/body injuries.
[2] Reframing is a technique taught in cognitive behavioural therapy (CBT) where people learn to identify and then shift their mindset when they encounter a challenging situation or experience. A study by Niknejad et al. (2018) found that this type of intervention can reduce pain and improve pain self-efficacy for managing pain.
[3] Mirror therapy is a technique that has been used since the 1990’s to treat phantom limb pain in persons with amputations and a systematic review by Colmenero et al. (2017) found that the technique can reduce phantom limb pain.
[4] Acupuncture produces effective results for people with various chronic conditions (Hu, et al., 2014). Acupuncture was shown to reduce phantom limb pain when used in conjunction with usual care, as opposed to just receiving usual care (Hu, et al., 2014).
Help keep this resource alive.
Click this Qualtrics link to fill out a survey on phantom pain so we can continue to grow the information and keep it up to date.